Coronary blood flow is a critical aspect of cardiovascular health, as it ensures the delivery of oxygen and nutrients to the heart muscle (myocardium). The coronary arteries, which branch off from the aorta, are responsible for this vital function.
Any disturbance in coronary blood flow can lead to severe consequences, such as ischemia, myocardial infarction, and heart failure. Understanding the factors that affect coronary blood flow is essential for preventing and managing cardiovascular diseases. This article explores these factors in detail, including anatomical, physiological, and pathological influences.
1. Anatomical Factors
Coronary Artery Anatomy
The coronary arteries include the left main coronary artery, which branches into the left anterior descending artery (LAD) and the left circumflex artery (LCx), and the right coronary artery (RCA). The anatomy of these arteries plays a significant role in blood flow. Variations in the branching patterns and the presence of congenital anomalies can affect how blood is distributed within the heart muscle.
Vessel Diameter and Length
The diameter and length of coronary vessels directly influence blood flow. Larger diameters allow for greater blood flow, while longer vessels can increase resistance and reduce flow. Changes in vessel diameter, such as those caused by atherosclerosis, can significantly impact coronary circulation.
Coronary Collateral Circulation
Collateral circulation refers to the network of tiny blood vessels that can bypass blockages in the main coronary arteries. The extent and efficiency of collateral circulation can vary among individuals and can significantly influence the ability of the heart to maintain adequate blood flow during obstructive coronary artery disease.
SEE ALSO: The 6 Best Natural Remedies for Blocked Coronary Arteries
2. Physiological Factors
Heart Rate and Contractility
Heart rate and myocardial contractility directly impact coronary blood flow. Increased heart rate and contractility raise the oxygen demand of the heart, requiring increased blood flow to meet this demand. However, excessively high heart rates can reduce the time available for coronary perfusion, particularly during diastole, when the majority of coronary blood flow occurs.
Aortic Pressure
Coronary perfusion pressure is largely determined by the pressure in the aorta, as the coronary arteries originate from the aortic root. Higher aortic pressures generally lead to increased coronary blood flow, while lower pressures can compromise perfusion.
Autoregulation
The coronary arteries have the ability to autoregulate blood flow, maintaining consistent perfusion despite changes in systemic blood pressure. This autoregulation is achieved through the dilation and constriction of coronary vessels in response to metabolic needs and pressure changes.
Endothelial Function
The endothelium, the inner lining of blood vessels, plays a crucial role in regulating coronary blood flow. Endothelial cells produce substances like nitric oxide (NO) that promote vasodilation, increasing blood flow. Endothelial dysfunction, often caused by conditions like hypertension and hyperlipidemia, can impair this regulation and reduce coronary blood flow.
Myocardial Oxygen Demand
The oxygen demand of the myocardium is a major determinant of coronary blood flow. Factors such as physical activity, emotional stress, and metabolic rate can influence myocardial oxygen consumption. The heart adjusts blood flow accordingly to meet these changing demands.
3. Pathological Factors
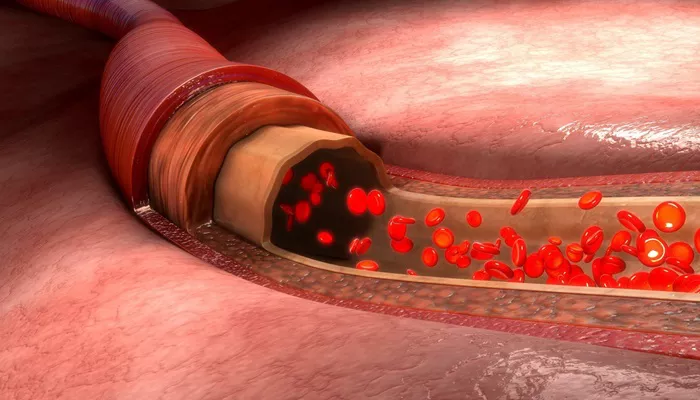
Atherosclerosis
Atherosclerosis, the buildup of plaques within the coronary arteries, is a leading cause of reduced coronary blood flow.
Plaques can obstruct blood flow directly or lead to plaque rupture and thrombosis, resulting in acute coronary syndromes.
The extent and severity of atherosclerosis are critical factors in determining coronary blood flow.
Coronary Artery Spasm
Coronary artery spasm, or vasospasm, can transiently reduce or block blood flow through the coronary arteries. This spasm can occur in the presence or absence of atherosclerosis and is often triggered by factors such as stress, smoking, and certain medications.
Thrombosis
Thrombosis refers to the formation of a blood clot within a coronary artery. This can occur due to plaque rupture or erosion in atherosclerosis. Thrombosis can lead to partial or complete occlusion of the artery, drastically reducing blood flow and potentially causing a myocardial infarction.
Inflammation
Inflammatory processes can affect coronary blood flow through several mechanisms. Inflammation can promote atherosclerosis, contribute to plaque instability, and lead to endothelial dysfunction. Conditions like chronic inflammatory diseases and acute infections can exacerbate these effects.
Microvascular Dysfunction
Microvascular dysfunction involves the smaller coronary vessels that are not visible on standard angiography. This condition can result from endothelial dysfunction, smooth muscle cell abnormalities, or increased vascular resistance. Microvascular dysfunction can significantly impair coronary blood flow, particularly in patients with conditions like diabetes and hypertension.
4. External Factors
Physical Activity
Physical activity has a profound impact on coronary blood flow. During exercise, the heart’s oxygen demand increases, prompting vasodilation of the coronary arteries and increased blood flow. Regular physical activity improves endothelial function and promotes the development of collateral circulation, enhancing overall coronary blood flow.
Diet and Nutrition
Diet and nutrition can influence coronary blood flow by affecting cardiovascular health. Diets high in saturated fats, trans fats, and cholesterol can promote atherosclerosis, while diets rich in fruits, vegetables, whole grains, and healthy fats can improve endothelial function and reduce inflammation.
Smoking
Smoking is a major risk factor for cardiovascular disease and negatively impacts coronary blood flow. It promotes atherosclerosis, endothelial dysfunction, and inflammation. Quitting smoking is essential for improving coronary artery health and restoring optimal blood flow.
Stress
Chronic stress can adversely affect coronary blood flow by increasing heart rate, blood pressure, and promoting inflammation. Stress management techniques, such as mindfulness, exercise, and adequate sleep, are important for maintaining healthy coronary circulation.
Medications
Certain medications can influence coronary blood flow. For example, beta-blockers reduce heart rate and myocardial oxygen demand, while nitrates promote vasodilation. Statins can improve endothelial function and reduce atherosclerosis progression. Understanding the effects of these medications is crucial for managing coronary artery disease.
Diagnostic And Therapeutic Approaches
Non-Invasive Imaging
Non-invasive imaging techniques, such as coronary computed tomography angiography (CTA) and magnetic resonance imaging (MRI), allow for the assessment of coronary anatomy and blood flow. These tools are valuable for diagnosing coronary artery disease and planning appropriate interventions.
Invasive Procedures
Invasive procedures, such as coronary angiography, provide detailed information about coronary anatomy and blood flow. Interventions like percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) can restore blood flow in obstructed arteries and improve patient outcomes.
Pharmacological Interventions
Pharmacological interventions aim to optimize coronary blood flow and manage underlying conditions. Medications like antiplatelets, anticoagulants, statins, and antihypertensives play a crucial role in preventing and treating coronary artery disease.
Conclusion
Coronary blood flow is influenced by a complex interplay of anatomical, physiological, pathological, and external factors.
Understanding these factors is essential for the prevention, diagnosis, and management of coronary artery disease. By addressing modifiable risk factors, such as diet, physical activity, smoking, and stress, and utilizing appropriate diagnostic and therapeutic interventions, healthcare providers can significantly improve coronary blood flow and cardiovascular outcomes for patients.