Hypertension, commonly known as high blood pressure, is a widespread health condition affecting millions worldwide.
While often associated with cardiovascular issues, hypertension can also have significant neurological consequences. One such severe complication is hypertensive encephalopathy, a life-threatening condition that requires immediate medical attention. Understanding the relationship between hypertension and encephalopathy is crucial for both prevention and effective management.
Pathophysiology of Hypertension
The development of hypertension involves multiple factors, including genetic predisposition, lifestyle choices, and environmental influences. Key mechanisms include increased cardiac output, elevated systemic vascular resistance, and changes in the renin-angiotensin-aldosterone system (RAAS). Chronic hypertension leads to structural and functional changes in the blood vessels, heart, and kidneys, contributing to the progression of the disease and its complications.
Hypertensive Crises
A hypertensive crisis is a severe elevation in blood pressure that can be classified into two categories: hypertensive urgency and hypertensive emergency. Hypertensive urgency involves extremely high blood pressure without evidence of target organ damage, whereas hypertensive emergency is characterized by severe hypertension with acute target organ damage, including hypertensive encephalopathy.
SEE ALSO: How HighSalt Intake Causes Hypertension
Hypertensive Encephalopathy: An Overview
Definition and Symptoms
Hypertensive encephalopathy is a neurological syndrome caused by a sudden and severe elevation in blood pressure, leading to cerebral edema (swelling of the brain) and increased intracranial pressure. Symptoms can include:
Severe headache
Nausea and vomiting
Altered mental status (confusion, agitation, delirium)
Visual disturbances (blurred vision, temporary blindness)
Seizures
Focal neurological deficits (weakness, numbness, difficulty speaking)
Pathogenesis
The pathogenesis of hypertensive encephalopathy involves the disruption of cerebral autoregulation, the mechanism by which the brain maintains stable blood flow despite changes in systemic blood pressure. In the setting of severe hypertension, this autoregulatory capacity is overwhelmed, leading to increased cerebral blood flow and capillary leakage.
The resulting vasogenic edema (fluid accumulation in the extracellular space) and increased intracranial pressure contribute to the clinical manifestations of hypertensive encephalopathy.
Mechanisms Linking Hypertension to Encephalopathy
Cerebral Autoregulation Failure
Under normal conditions, cerebral autoregulation ensures that blood flow to the brain remains constant despite fluctuations in systemic blood pressure. This is achieved through the constriction and dilation of cerebral blood vessels. In chronic hypertension, the autoregulatory curve shifts, meaning higher blood pressure levels are required to maintain adequate cerebral perfusion. However, in a hypertensive crisis, this compensatory mechanism fails, leading to excessive blood flow to the brain and the breakdown of the blood-brain barrier.
Endothelial Dysfunction
The endothelium, a thin layer of cells lining the blood vessels, plays a critical role in vascular health by regulating vascular tone, blood flow, and permeability. Chronic hypertension can cause endothelial dysfunction, characterized by reduced nitric oxide availability, increased oxidative stress, and inflammation. This dysfunction contributes to impaired cerebral autoregulation and increased susceptibility to hypertensive encephalopathy.
Blood-Brain Barrier Disruption
The blood-brain barrier (BBB) is a selective permeability barrier that protects the brain from harmful substances in the bloodstream while allowing essential nutrients to pass through. Severe hypertension can compromise the integrity of the BBB, leading to leakage of fluid and proteins into the brain parenchyma. This results in vasogenic edema and increased intracranial pressure, key features of hypertensive encephalopathy.
Neurohormonal Activation
Hypertension is associated with the activation of various neurohormonal systems, including the sympathetic nervous system and the RAAS. Elevated levels of catecholamines (epinephrine and norepinephrine) and angiotensin II can cause vasoconstriction and increased vascular permeability, exacerbating cerebral edema and contributing to the development of hypertensive encephalopathy.
Clinical Presentation And Diagnosis
Clinical Features
Patients with hypertensive encephalopathy typically present with a constellation of neurological symptoms that may evolve rapidly. The clinical presentation can vary but often includes:
Headache: Severe and throbbing, often described as the worst headache of the patient’s life.
Altered Mental Status: Ranging from confusion and agitation to lethargy and coma.
Visual Disturbances: Blurred vision, scotomata (blind spots), and transient visual loss.
Seizures: Generalized or focal, occurring in up to 25% of cases.
Focal Neurological Deficits: Such as hemiparesis (weakness on one side of the body) or aphasia (difficulty speaking).
Diagnostic Evaluation
The diagnosis of hypertensive encephalopathy is primarily clinical, supported by a thorough history, physical examination, and appropriate diagnostic tests. Key elements of the diagnostic workup include:
Blood Pressure Measurement: Confirming severe hypertension, often with systolic BP >180 mm Hg and/or diastolic BP >120 mm Hg.
Neurological Examination: Assessing mental status, cranial nerve function, motor and sensory deficits, and signs of increased intracranial pressure.
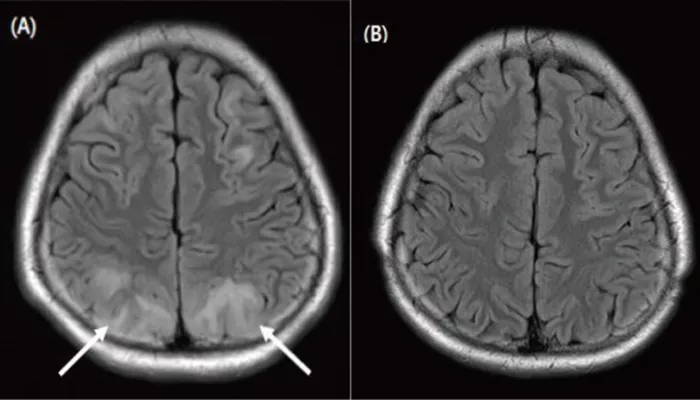
Imaging Studies: Brain imaging (CT or MRI) can help rule out other causes of neurological symptoms, such as stroke or intracranial hemorrhage. MRI may show findings consistent with vasogenic edema, particularly in the posterior regions of the brain (posterior reversible encephalopathy syndrome – PRES).
Laboratory Tests: Including renal function tests, electrolyte levels, and assessment for secondary causes of hypertension.
Management of Hypertensive Encephalopathy
Immediate Goals
The primary goals in the management of hypertensive encephalopathy are to rapidly lower blood pressure to a safer level and to prevent further neurological damage. This typically involves:
Intravenous Antihypertensive Therapy: Medications such as labetalol, nicardipine, or nitroprusside are commonly used due to their rapid onset and ease of titration.
Monitoring and Supportive Care: Continuous monitoring of blood pressure, neurological status, and vital signs is essential. Supportive measures may include oxygen therapy, seizure management, and control of intracranial pressure.
Long-Term Management
Once the acute crisis is stabilized, long-term management focuses on controlling hypertension and preventing recurrence.
This may involve:
Lifestyle Modifications: Dietary changes (reducing salt intake, increasing fruits and vegetables), regular physical activity, weight management, and smoking cessation.
Pharmacotherapy: A tailored regimen of antihypertensive medications to achieve and maintain target blood pressure levels. Common classes of drugs include ACE inhibitors, angiotensin II receptor blockers (ARBs), calcium channel blockers, diuretics, and beta-blockers.
Regular Monitoring: Frequent follow-up visits to monitor blood pressure, assess adherence to treatment, and adjust medications as needed.
Prognosis And Complications
Prognosis
With prompt recognition and appropriate treatment, the prognosis for patients with hypertensive encephalopathy is generally favorable. Most patients experience significant improvement in symptoms within 24-48 hours of initiating treatment. However, delayed or inadequate management can lead to permanent neurological damage or death.
Complications
Potential complications of hypertensive encephalopathy include:
Cerebral Hemorrhage: Severe hypertension can lead to rupture of cerebral blood vessels, resulting in intracerebral hemorrhage.
Stroke: Both ischemic and hemorrhagic strokes can occur due to the effects of uncontrolled hypertension on the cerebral vasculature.
Chronic Kidney Disease: Prolonged hypertension can damage the kidneys, leading to chronic kidney disease and further complicating blood pressure management.
Cardiovascular Events: Patients with hypertensive encephalopathy are at increased risk for myocardial infarction, heart failure, and other cardiovascular events.
Conclusion
Hypertensive encephalopathy is a serious and potentially life-threatening complication of severe hypertension.
Understanding the mechanisms by which hypertension causes encephalopathy is essential for early recognition, prompt treatment, and effective long-term management. By addressing the underlying hypertension and implementing appropriate preventive measures, the risk of hypertensive encephalopathy and its associated complications can be significantly reduced.