Familial Combined Hyperlipidemia (FCHL) is a common genetic disorder that significantly increases the risk of cardiovascular disease (CVD) due to abnormal levels of lipids in the blood. It is characterized by elevated levels of triglycerides, low-density lipoprotein cholesterol (LDL-C), and apolipoprotein B (ApoB), which can lead to premature atherosclerosis and coronary artery disease (CAD). FCHL affects approximately 1 in 100 to 1 in 200 people, making it a prevalent cause of inherited lipid disorders.
Pathophysiology of Familial Combined Hyperlipidemia
The pathophysiology of FCHL is complex and multifactorial, involving genetic and environmental factors. The disorder is polygenic, meaning multiple genes contribute to its development. Key genes implicated in FCHL include those involved in lipid metabolism, such as APOA1, APOA5, APOC3, LPL, and USF1.
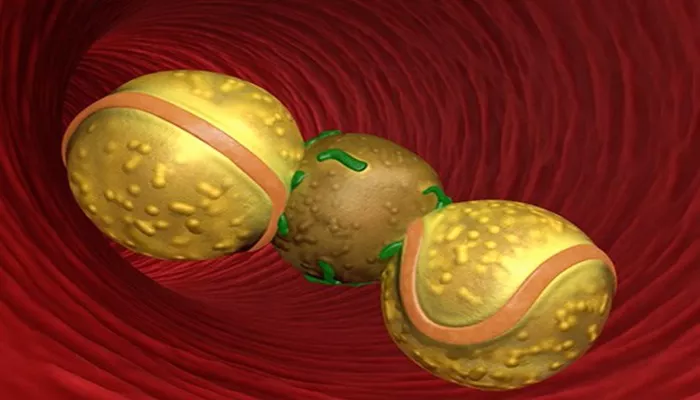
Lipid Metabolism Abnormalities: Individuals with FCHL exhibit overproduction of very low-density lipoprotein (VLDL) particles by the liver, resulting in elevated triglyceride levels. These VLDL particles are then converted to LDL-C, leading to increased levels of LDL-C in the blood.
Apolipoprotein B Overproduction: ApoB is a primary component of VLDL and LDL particles. Overproduction of ApoB leads to an increase in the number of atherogenic lipoprotein particles, which can deposit cholesterol in arterial walls and form plaques, contributing to atherosclerosis.
Insulin Resistance: Many individuals with FCHL exhibit insulin resistance, which exacerbates dyslipidemia by increasing hepatic VLDL production and decreasing lipoprotein lipase activity, an enzyme essential for triglyceride breakdown.
see also: What Labs Show Hyperlipidemia?
Clinical Manifestations of Familial Combined Hyperlipidemia
FCHL presents a spectrum of lipid abnormalities and clinical manifestations:
Lipid Profile: The lipid profile of individuals with FCHL is variable but typically includes elevated triglycerides, increased LDL-C, and normal or low high-density lipoprotein cholesterol (HDL-C). Elevated ApoB levels are a hallmark of FCHL.
Cardiovascular Disease: Due to the elevated atherogenic lipoproteins, individuals with FCHL have a higher risk of developing CVD, including CAD, myocardial infarction, and peripheral artery disease. The risk of premature CVD is significantly elevated in affected individuals.
Physical Findings: Unlike other lipid disorders, FCHL is not associated with physical findings such as xanthomas (cholesterol deposits in the skin) or corneal arcus (cholesterol deposits in the cornea).
Diagnosis of Familial Combined Hyperlipidemia
Diagnosing FCHL involves a combination of clinical evaluation, family history, and laboratory testing:
Lipid Profile: A fasting lipid profile is essential for diagnosing FCHL. Elevated triglycerides, LDL-C, and ApoB levels with normal or low HDL-C are indicative of FCHL.
Family History: A thorough family history can reveal a pattern of dyslipidemia and premature CVD, supporting the diagnosis of FCHL. Affected individuals often have first-degree relatives with similar lipid abnormalities or CVD.
Genetic Testing: While there is no single genetic test for FCHL due to its polygenic nature, genetic testing can identify mutations in genes associated with lipid metabolism that may contribute to the disorder.
Exclusion of Secondary Causes: Secondary causes of dyslipidemia, such as hypothyroidism, diabetes, and liver disease, should be excluded to confirm a diagnosis of FCHL.
Management of Familial Combined Hyperlipidemia
Managing FCHL involves lifestyle modifications and pharmacological interventions aimed at reducing lipid levels and minimizing CVD risk:
Lifestyle Modifications:
Diet: A heart-healthy diet low in saturated fats, trans fats, and cholesterol is recommended. Increasing intake of omega-3 fatty acids, fiber, and plant sterols can help improve lipid profiles.
Exercise: Regular physical activity can enhance lipid metabolism, reduce triglycerides, and improve insulin sensitivity.
Weight Management: Achieving and maintaining a healthy weight is crucial, as obesity can exacerbate lipid abnormalities.
Pharmacological Treatment:
Statins: Statins are the first-line treatment for reducing LDL-C levels and decreasing CVD risk. They inhibit HMG-CoA reductase, an enzyme involved in cholesterol synthesis.
Fibrates: Fibrates are effective in lowering triglycerides and increasing HDL-C levels. They activate peroxisome proliferator-activated receptors (PPARs), which regulate lipid metabolism.
Ezetimibe: Ezetimibe inhibits intestinal absorption of cholesterol, reducing LDL-C levels.
PCSK9 Inhibitors: These monoclonal antibodies enhance the clearance of LDL-C from the bloodstream by inhibiting the protein PCSK9, which degrades LDL receptors.
Omega-3 Fatty Acid Supplements: High doses of omega-3 fatty acids can reduce triglyceride levels.
Prognosis and Long-Term Management
The prognosis for individuals with FCHL depends on the effectiveness of lipid-lowering therapy and adherence to lifestyle modifications. Early detection and aggressive management are crucial for preventing CVD and improving long-term outcomes. Regular monitoring of lipid levels, liver function, and glucose metabolism is essential for adjusting treatment and minimizing side effects.
Conclusion
Familial Combined Hyperlipidemia is a common and complex genetic disorder characterized by elevated levels of triglycerides, LDL-C, and ApoB. It significantly increases the risk of cardiovascular disease and requires a comprehensive management approach involving lifestyle modifications and pharmacological treatment. Early diagnosis and aggressive intervention are key to reducing the risk of premature CVD and improving the quality of life for affected individuals.