Heart failure is a chronic and progressive condition that significantly impacts the heart’s ability to pump blood effectively.
This condition can lead to a range of serious complications that affect the entire body. In this article, we will explore how heart failure hinders normal circulatory functioning and the subsequent effects on various body systems.
The Mechanism of Normal Circulatory Function
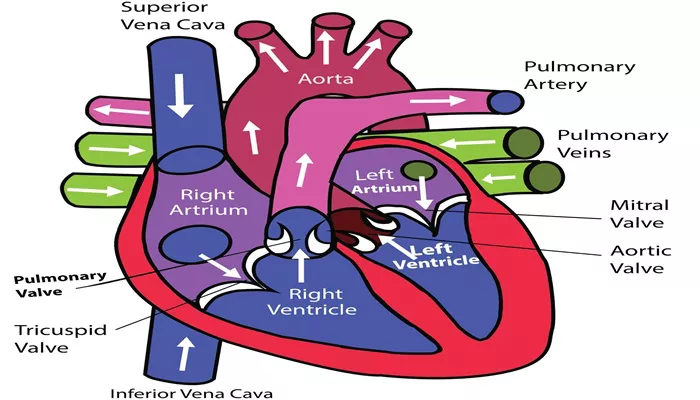
The circulatory system is essential for delivering oxygen and nutrients to tissues and organs, as well as removing waste products from the body. The heart is the central component of this system, and it functions through a coordinated series of contractions that ensure blood flow throughout the body. The right side of the heart receives deoxygenated blood from the body and pumps it to the lungs, where it gets oxygenated. The left side of the heart then pumps the oxygen-rich blood to the rest of the body.
How Does Heart Failure Hinder Normal Circulatory Functioning?
1. Heart Failure: A Disruption in the System
Heart failure occurs when the heart muscle becomes weakened or damaged, leading to a reduced ability to pump blood effectively. This condition can result from various causes, including coronary artery disease, hypertension, myocardial infarction, cardiomyopathy, and valvular heart disease. Regardless of the underlying cause, the outcome is a diminished cardiac output and impaired circulation.
SEE ALSO: What Happens to Preload in Heart Failure?
2. Reduced Cardiac Output
One of the primary ways heart failure hinders normal circulatory functioning is through a reduction in cardiac output.
Cardiac output is the volume of blood the heart pumps per minute, and it is determined by both the heart rate and the stroke volume (the amount of blood pumped with each beat). In heart failure, the heart’s pumping efficiency is compromised, leading to a decreased stroke volume and, consequently, a lower cardiac output. This reduction means that less blood is available to supply the body’s tissues with essential oxygen and nutrients.
3. Increased Ventricular Filling Pressures
In heart failure, the heart’s ventricles often become stiff and less compliant, making it more difficult for them to fill with blood during diastole (the relaxation phase of the cardiac cycle). This leads to increased pressures within the ventricles and atria, causing blood to back up into the veins and capillaries. This backup can result in congestion and fluid accumulation in various parts of the body, contributing to symptoms such as edema (swelling), particularly in the legs and ankles, and pulmonary congestion, leading to shortness of breath.
4. Neurohormonal Activation
Heart failure triggers a series of compensatory mechanisms aimed at maintaining adequate blood flow and pressure. One of the primary responses is the activation of the sympathetic nervous system, which increases heart rate and contractility.
Additionally, the renin-angiotensin-aldosterone system (RAAS) is activated, leading to vasoconstriction (narrowing of blood vessels) and sodium and water retention. While these mechanisms initially help support circulation, over time, they place additional strain on the heart and exacerbate heart failure symptoms.
5. Vasoconstriction and Increased Afterload
Vasoconstriction, or the narrowing of blood vessels, is a common response in heart failure. This process increases afterload, which is the resistance the heart must overcome to eject blood. An elevated afterload places additional stress on the weakened heart, further reducing its pumping efficiency. The increased resistance also leads to higher blood pressure, compounding the challenges of maintaining effective circulation.
6. Fluid Retention and Edema
The activation of the RAAS in heart failure results in the retention of sodium and water by the kidneys. This fluid retention increases blood volume and contributes to the development of edema. Edema can occur in various parts of the body, including the legs, ankles, and abdomen. In severe cases, fluid may accumulate in the lungs, leading to pulmonary edema, a condition characterized by difficulty breathing and reduced oxygen exchange.
7. Pulmonary Congestion
In left-sided heart failure, the left ventricle’s inability to pump blood effectively leads to increased pressure in the left atrium and pulmonary veins. This pressure buildup causes fluid to leak into the lung tissues and air sacs, resulting in pulmonary congestion. Patients with pulmonary congestion often experience shortness of breath, particularly when lying flat (orthopnea) or during physical activity. Severe pulmonary congestion can lead to acute pulmonary edema, a life-threatening condition requiring immediate medical intervention.
8. Decreased Organ Perfusion
As heart failure progresses, the reduced cardiac output and impaired circulation result in decreased perfusion of vital organs, including the kidneys, liver, and brain. Reduced kidney perfusion can lead to renal dysfunction or failure, further complicating fluid balance and electrolyte regulation. Impaired liver perfusion can cause hepatic congestion and dysfunction. Decreased cerebral perfusion may result in cognitive impairment, dizziness, and an increased risk of stroke.
9. Metabolic and Nutritional Imbalances
Heart failure can disrupt normal metabolic and nutritional processes. Reduced blood flow to the gastrointestinal tract can impair digestion and nutrient absorption, leading to malnutrition and weight loss. Additionally, the increased metabolic demands of the failing heart can deplete the body’s energy reserves, exacerbating fatigue and weakness.
Impact on Physical Activity And Quality of Life
The symptoms of heart failure, including fatigue, shortness of breath, and edema, can significantly impact a patient’s ability to engage in physical activity and perform daily tasks. The reduced exercise tolerance and physical limitations often lead to a decline in quality of life. Patients may experience depression, anxiety, and social isolation due to their inability to participate in activities they once enjoyed.
Management of Heart Failure
While heart failure is a chronic condition with no cure, various treatments and lifestyle modifications can help manage symptoms and improve quality of life. Medications such as diuretics, ACE inhibitors, beta-blockers, and aldosterone antagonists are commonly prescribed to manage fluid retention, reduce blood pressure, and support heart function.
Lifestyle changes, including a low-sodium diet, regular physical activity, and weight management, are also crucial components of heart failure management.
Advanced Therapies and Interventions
For patients with severe heart failure, advanced therapies may be necessary. These can include implantable devices such as pacemakers and defibrillators, which help regulate heart rhythm and prevent sudden cardiac arrest. In some cases, patients may require surgical interventions such as coronary artery bypass grafting (CABG) or heart valve repair or replacement. For those with end-stage heart failure, heart transplantation may be considered as a last resort.
Conclusion
Heart failure significantly hinders normal circulatory functioning through a combination of reduced cardiac output, increased ventricular filling pressures, neurohormonal activation, vasoconstriction, fluid retention, and decreased organ perfusion. These mechanisms lead to a range of symptoms and complications that affect multiple body systems. While heart failure is a serious and chronic condition, appropriate medical management and lifestyle modifications can help improve symptoms, enhance quality of life, and reduce the risk of hospitalization and adverse outcomes.