Hyperlipidemia, a condition characterized by elevated levels of lipids (fats) in the blood, is a major risk factor for cardiovascular disease and other systemic health issues. This condition often manifests as elevated cholesterol and triglyceride levels and can have profound effects on various body systems. Understanding the impact of hyperlipidemia on the body is crucial for effective management and prevention of related health problems.
This article delves into the effects of hyperlipidemia on the body, including its role in cardiovascular disease, its impact on other organs, and its contribution to systemic health issues. Additionally, it will touch upon testing for pulmonary hypertension, a condition often linked to hyperlipidemia.
The Pathophysiology of Hyperlipidemia
Hyperlipidemia involves an abnormal increase in lipid levels in the bloodstream, primarily cholesterol and triglycerides. The main types of lipids include:
Low-Density Lipoprotein (LDL) Cholesterol: Often referred to as “bad” cholesterol, high levels of LDL can lead to plaque buildup in arterial walls.
High-Density Lipoprotein (HDL) Cholesterol: Known as “good” cholesterol, HDL helps remove LDL from the bloodstream. Low levels of HDL are also problematic.
Triglycerides: Elevated triglycerides are associated with increased risk of cardiovascular disease and metabolic syndrome.
Hyperlipidemia can be caused by genetic factors (primary hyperlipidemia) or result from lifestyle and dietary factors (secondary hyperlipidemia). Both forms can lead to significant health issues if not managed properly.
What Does Hyperlipidemia Do to The Body?
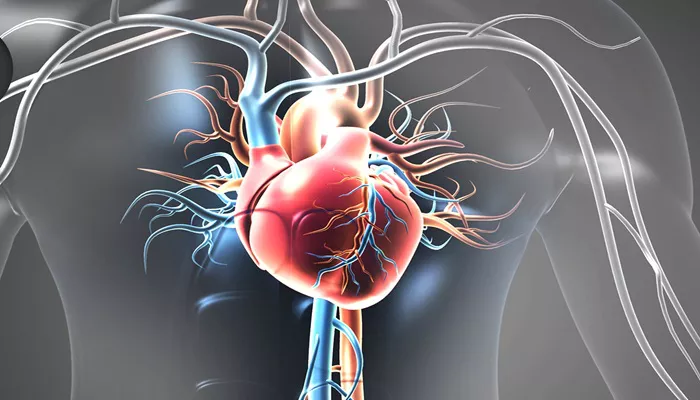
1. Impact of Hyperlipidemia on the Cardiovascular System
Atherosclerosis
One of the most direct and dangerous consequences of hyperlipidemia is atherosclerosis, a condition where fatty deposits build up in the walls of arteries. This buildup can form plaques, leading to narrowing and hardening of the arteries. Key points include:
Plaque Formation: High levels of LDL cholesterol contribute to plaque formation in arterial walls. These plaques can restrict blood flow and cause complications.
Increased Risk of Coronary Artery Disease (CAD): Atherosclerosis increases the risk of CAD, which can lead to angina, myocardial infarction (heart attack), and heart failure.
SEE ALSO: How to Explain Hyperlipidemia to A Patient
Hypertension
Hyperlipidemia is closely linked with hypertension (high blood pressure). The process of atherosclerosis increases arterial resistance, which in turn elevates blood pressure. Persistent hypertension can exacerbate the damage to arterial walls and accelerate cardiovascular disease progression.
Peripheral Artery Disease (PAD)
Elevated lipid levels can also affect the peripheral arteries, leading to PAD. This condition involves reduced blood flow to the limbs, causing symptoms like claudication (pain or cramping in the legs during exercise). PAD increases the risk of heart attack and stroke.
Stroke
The risk of stroke is elevated in individuals with hyperlipidemia due to the potential for atherosclerosis and emboli formation. A stroke occurs when blood flow to a part of the brain is blocked or reduced, leading to brain cell damage.
2. Effects on the Endocrine System
Insulin Resistance and Diabetes
Hyperlipidemia is often associated with insulin resistance, a condition where the body’s cells become less responsive to insulin. This can lead to type 2 diabetes, a chronic disease with its own set of complications. Elevated triglycerides, in particular, are a significant risk factor for developing insulin resistance.
Metabolic Syndrome
Hyperlipidemia is a component of metabolic syndrome, a cluster of conditions that includes abdominal obesity, hypertension, and dysglycemia (abnormal blood glucose levels). Metabolic syndrome increases the risk of cardiovascular disease, diabetes, and stroke.
3. Impact on the Liver
Non-Alcoholic Fatty Liver Disease (NAFLD)
High levels of triglycerides and cholesterol can lead to the accumulation of fat in the liver, resulting in NAFLD. This condition can progress to non-alcoholic steatohepatitis (NASH), which involves liver inflammation and can lead to cirrhosis or liver cancer.
Liver Dysfunction
Persistent hyperlipidemia can impair liver function, affecting the organ’s ability to metabolize fats and process other nutrients. This dysfunction can result in elevated liver enzymes and other metabolic disturbances.
4. Effects on the Renal System
Chronic Kidney Disease (CKD)
Hyperlipidemia contributes to the development and progression of CKD. The process of atherosclerosis can affect the renal arteries, leading to reduced blood flow and kidney function. Additionally, lipid deposits can contribute to kidney damage and inflammation.
Proteinuria
Increased lipid levels can also cause proteinuria (the presence of excess protein in the urine), a marker of kidney damage.
Proteinuria is a common complication in patients with diabetes and hypertension, both of which are associated with hyperlipidemia.
5. Impact on the Nervous System
Cognitive Decline
Chronic hyperlipidemia has been linked to cognitive decline and neurodegenerative diseases. Elevated cholesterol levels may contribute to the development of Alzheimer’s disease and other forms of dementia by promoting inflammation and oxidative stress in the brain.
Peripheral Neuropathy
Hyperlipidemia, particularly when associated with diabetes, can cause peripheral neuropathy. This condition involves damage to the peripheral nerves, leading to symptoms such as pain, tingling, and numbness in the extremities.
Testing for Pulmonary Hypertension
Pulmonary hypertension (PH) is a serious condition characterized by elevated blood pressure in the pulmonary arteries, which can be exacerbated by underlying conditions such as hyperlipidemia. Testing for PH is crucial for timely diagnosis and management. The methods for diagnosing pulmonary hypertension include:
Clinical Evaluation
Symptoms of PH may include shortness of breath, fatigue, chest pain, and swelling of the ankles or legs. A thorough clinical evaluation is essential to assess these symptoms and their potential underlying causes.
Echocardiography
Echocardiography is a non-invasive imaging technique used to estimate pulmonary artery pressure. This test involves using ultrasound waves to create images of the heart and blood vessels. Key points include:
Tricuspid Regurgitant Jet Velocity: Measurement of the velocity of blood flow across the tricuspid valve can estimate the pressure in the pulmonary artery.
Right Heart Dimensions: Assessment of the size and function of the right heart chambers provides additional information about pulmonary pressures.
Right Heart Catheterization
Right heart catheterization is the gold standard for directly measuring pulmonary artery pressure. This invasive procedure involves inserting a catheter into the right side of the heart and pulmonary artery to obtain accurate pressure readings. It is typically performed when non-invasive tests are inconclusive or when a precise diagnosis is required.
Pulmonary Function Tests (PFTs)
PFTs assess lung function and can help identify underlying respiratory conditions contributing to PH. These tests measure lung volumes, capacities, and gas exchange efficiency.
Chest Imaging
Imaging techniques such as chest X-rays or computed tomography (CT) scans can be used to evaluate the structure of the lungs and pulmonary vessels. These tests help rule out other causes of symptoms and provide additional information about the extent of pulmonary changes.
Management And Prevention
Managing hyperlipidemia involves a combination of lifestyle changes, medications, and regular monitoring:
Lifestyle Modifications
Diet: Adopting a heart-healthy diet low in saturated fats, trans fats, and cholesterol can help reduce lipid levels. Emphasize fruits, vegetables, whole grains, and lean proteins.
Exercise: Regular physical activity helps improve lipid profiles and overall cardiovascular health. Aim for at least 150 minutes of moderate-intensity exercise per week.
Weight Management: Maintaining a healthy weight can improve lipid levels and reduce the risk of associated conditions like diabetes and hypertension.
Medications
Statins: Statins are commonly prescribed to lower LDL cholesterol levels and reduce cardiovascular risk.
Fibrates: These medications help lower triglyceride levels and can be used in combination with statins.
Ezetimibe: This drug reduces cholesterol absorption in the intestines and can be used alone or with statins.
Conclusion
Hyperlipidemia has a wide range of effects on the body, from cardiovascular damage and metabolic disturbances to liver and renal complications. Its impact extends to various systems, highlighting the importance of early detection, effective management, and preventive measures. Testing for conditions like pulmonary hypertension is crucial for individuals with hyperlipidemia, as it can be exacerbated by elevated lipid levels.