Arrhythmias, or irregular heartbeats, can range from harmless to life-threatening. Understanding which types of arrhythmias pose the greatest risk is crucial for both medical professionals and patients. This article delves into the most dangerous form of arrhythmia, the mechanisms behind it, symptoms, risk factors, and treatment options.
Understanding Arrhythmias
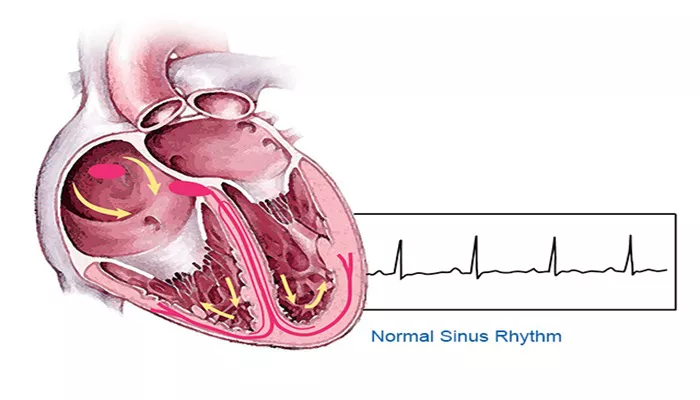
An arrhythmia occurs when the heart’s electrical impulses, which coordinate heartbeats, do not function correctly. This can cause the heart to beat too fast (tachycardia), too slow (bradycardia), or irregularly. While many arrhythmias are benign, others can significantly impair heart function and increase the risk of sudden cardiac death.
What Makes An Arrhythmia Life-Threatening?
Arrhythmias become life-threatening when they interfere significantly with the heart’s ability to pump blood. This can lead to insufficient blood flow to the brain and other vital organs, causing cardiac arrest or stroke. The most life-threatening arrhythmias often originate in the ventricles, the heart’s main pumping chambers.
The Most Life-Threatening Arrhythmia: Ventricular Fibrillation
Ventricular Fibrillation (VFib) is widely regarded as the most life-threatening arrhythmia. It is a chaotic and erratic firing of impulses from the ventricles, causing them to quiver rather than contract in a coordinated manner. This results in the cessation of effective blood flow, leading to a rapid loss of consciousness and sudden cardiac arrest.
SEE ALSO: How to Stop Sinus Arrhythmia
Causes of Ventricular Fibrillation
Several factors can trigger VFib, including:
Coronary Artery Disease (CAD): The most common cause of VFib, CAD narrows or blocks the coronary arteries, reducing blood flow to the heart muscle.
Heart Attack: A heart attack can damage the heart muscle, leading to electrical instability and VFib.
Cardiomyopathy: Diseases of the heart muscle can alter its structure and function, increasing the risk of VFib.
Electrolyte Imbalances: Abnormal levels of electrolytes such as potassium or magnesium can disrupt the heart’s electrical activity.
Drug Overdose or Toxicity: Certain drugs can affect the heart’s electrical conduction system, leading to VFib.
Severe Heart Failure: Weakening of the heart muscle can predispose to VFib.
Symptoms of Ventricular Fibrillation
VFib symptoms are severe and sudden, often leading to immediate collapse. They include:
Sudden Loss of Consciousness: Due to a sudden drop in blood flow to the brain.
No Pulse: The heart is not pumping blood effectively.
No Breathing: The cessation of effective circulation affects respiration.
Chest Pain or Discomfort: May precede the onset of VFib in some cases.
Diagnosing Ventricular Fibrillation
VFib is usually diagnosed in emergency situations through an electrocardiogram (ECG). The ECG will show rapid, erratic electrical activity in the ventricles. Additional tests to determine the underlying cause may include:
Blood Tests: To check for electrolyte imbalances or heart enzymes indicative of a heart attack.
Echocardiogram: To assess heart function and structure.
Coronary Angiography: To check for blockages in the coronary arteries.
Treatment And Management of Ventricular Fibrillation
Immediate treatment of VFib is crucial and involves:
Immediate Response
Cardiopulmonary Resuscitation (CPR): To maintain blood flow to vital organs until further treatment can be administered.
Defibrillation: The use of an automated external defibrillator (AED) to deliver an electric shock to restore normal heart rhythm.
Hospital Treatment
Medications: Drugs like antiarrhythmics can help stabilize the heart’s rhythm.
Implantable Cardioverter-Defibrillator (ICD): A device implanted in patients at high risk of VFib to monitor heart rhythm and deliver shocks if needed.
Cardiac Ablation: A procedure to destroy areas of heart tissue causing abnormal rhythms.
Long-Term Management
Managing underlying conditions and lifestyle changes are crucial for preventing recurrence. This may include:
Medications: Long-term use of beta-blockers, antiarrhythmics, or anticoagulants.
Lifestyle Modifications: Dietary changes, regular exercise, and avoiding smoking and excessive alcohol.
Regular Monitoring: Frequent check-ups with a cardiologist to monitor heart health and adjust treatments as necessary.
Preventing Ventricular Fibrillation
Preventing VFib involves managing risk factors and underlying health conditions:
Heart Health: Controlling high blood pressure, cholesterol, and diabetes.
Healthy Lifestyle: Maintaining a balanced diet, regular exercise, and avoiding tobacco and excessive alcohol.
Medications: Adhering to prescribed medications for heart conditions.
Regular Check-ups: Routine medical examinations to monitor and manage potential risk factors.
Conclusion
Ventricular Fibrillation is the most life-threatening type of arrhythmia due to its potential to cause sudden cardiac arrest.
Understanding the causes, symptoms, and treatment options is essential for managing this condition and improving patient outcomes. Prevention through lifestyle changes and managing underlying conditions plays a crucial role in reducing the risk of VFib.