Tachycardia is a condition characterized by an abnormally fast heart rate, typically defined as a heart rate exceeding 100 beats per minute in adults. This condition can arise from various underlying causes, and its manifestation on an electrocardiogram (ECG) can take different forms. Understanding the types of tachycardia on ECG is crucial for accurate diagnosis and effective management. This article delves into the various types of tachycardia that can be identified on an ECG, providing a detailed overview of their characteristics, underlying mechanisms, and clinical significance.
What Is Tachycardia?
Tachycardia refers to a heart rate that is faster than normal, usually more than 100 beats per minute. It can occur due to various reasons, including physiological responses to stress, fever, or exercise, as well as pathological conditions like cardiac arrhythmias. Tachycardia can be classified into different types based on its origin within the heart’s conduction system.
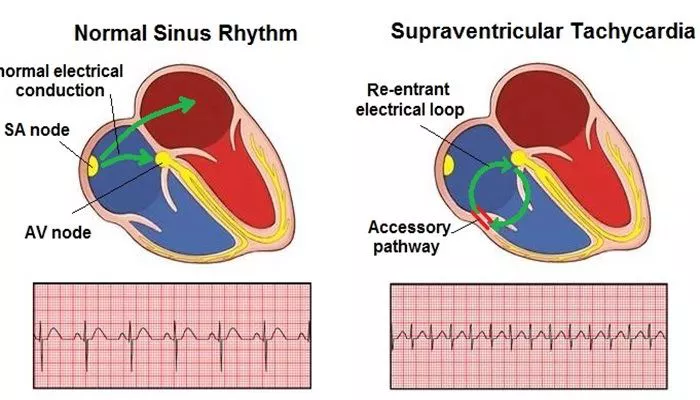
The heart’s electrical conduction system includes the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, and Purkinje fibers, which work together to coordinate the heart’s rhythm. When abnormalities occur in this system, they can lead to different forms of tachycardia, which are identifiable on an ECG.
Types of Tachycardia on ECG
Sinus Tachycardia
Definition and Characteristics: Sinus tachycardia is a condition where the heart’s natural pacemaker, the sinoatrial (SA) node, generates electrical impulses at a faster rate than normal. On an ECG, sinus tachycardia is characterized by a regular rhythm with a heart rate greater than 100 beats per minute. The P waves are upright in leads I, II, and aVF, and each P wave is followed by a QRS complex, indicating that the atria and ventricles are depolarizing in a coordinated manner.
Causes: Sinus tachycardia can be a normal physiological response to stress, exercise, fever, pain, or anxiety. It can also result from conditions such as hyperthyroidism, anemia, heart failure, or dehydration.
Clinical Significance: While sinus tachycardia is often benign and self-limiting, persistent or inappropriate sinus tachycardia may require further evaluation to identify and treat the underlying cause.
SEE ALSO: Why Does Caffeine Affect Blood Pressure?
Atrial Tachycardia
Definition and Characteristics: Atrial tachycardia is an arrhythmia that originates in the atria but outside the SA node. On an ECG, atrial tachycardia typically presents with a heart rate between 150 and 250 beats per minute. The P waves may have an abnormal morphology depending on the location of the ectopic focus within the atria, and the P-R interval may be shorter or longer than normal.
Causes: Atrial tachycardia can occur due to structural heart disease, electrolyte imbalances, or as a complication of heart surgery. It may also be idiopathic, with no identifiable cause.
Clinical Significance: Atrial tachycardia can be associated with symptoms such as palpitations, dizziness, or shortness of breath. It may lead to more serious arrhythmias if left untreated, particularly in individuals with underlying heart disease.
Supraventricular Tachycardia (SVT)
Definition and Characteristics: Supraventricular tachycardia (SVT) is a term that encompasses a group of arrhythmias that originate above the ventricles. The most common types of SVT include atrioventricular nodal reentrant tachycardia (AVNRT) and atrioventricular reciprocating tachycardia (AVRT). On an ECG, SVT is characterized by a regular, narrow QRS complex tachycardia with a heart rate typically between 150 and 250 beats per minute. P waves may be absent, buried in the QRS complex, or retrograde.
Causes: SVT can be triggered by stress, caffeine, alcohol, or certain medications. It can also occur in the setting of congenital heart conditions such as Wolff-Parkinson-White (WPW) syndrome, which is associated with AVRT.
Clinical Significance: SVT is often symptomatic, causing palpitations, chest discomfort, or syncope. Although not usually life-threatening, recurrent episodes may require medical intervention to prevent complications.
Ventricular Tachycardia (VT)
Definition and Characteristics: Ventricular tachycardia (VT) is an arrhythmia originating from the ventricles. On an ECG, VT is characterized by a wide QRS complex tachycardia with a heart rate typically between 120 and 250 beats per minute.
The rhythm may be regular or slightly irregular, and P waves are usually absent or dissociated from the QRS complexes.
Causes: VT is commonly associated with ischemic heart disease, cardiomyopathy, electrolyte disturbances, and structural heart abnormalities. It can also occur in the setting of prolonged QT syndrome or as a result of drug toxicity.
Clinical Significance: VT is a potentially life-threatening arrhythmia that can lead to hemodynamic instability, syncope, or sudden cardiac death. Immediate medical intervention is often required to prevent progression to ventricular fibrillation, a more dangerous arrhythmia.
Ventricular Fibrillation (VF)
Definition and Characteristics: Ventricular fibrillation (VF) is a chaotic and disorganized electrical activity in the ventricles that results in an absence of effective cardiac output. On an ECG, VF is characterized by rapid, irregular, and erratic waveforms without identifiable P waves, QRS complexes, or T waves.
Causes: VF is most commonly associated with acute myocardial infarction (heart attack) but can also occur in the context of severe electrolyte imbalances, drug toxicity, or primary electrical abnormalities such as Brugada syndrome.
Clinical Significance: VF is a medical emergency and is the leading cause of sudden cardiac death. Immediate defibrillation and advanced cardiac life support (ACLS) are required to restore normal rhythm and prevent death.
Atrial Fibrillation (AF) with Rapid Ventricular Response
Definition and Characteristics: Atrial fibrillation (AF) is the most common sustained arrhythmia, characterized by rapid and irregular electrical activity in the atria. When AF occurs with a rapid ventricular response (RVR), it can lead to tachycardia.
On an ECG, AF with RVR presents as an irregularly irregular rhythm with no discernible P waves and variable R-R intervals.
The ventricular rate is typically greater than 100 beats per minute.
Causes: AF with RVR can be triggered by conditions such as hypertension, valvular heart disease, heart failure, or hyperthyroidism.
It can also occur in otherwise healthy individuals due to stress, alcohol, or excessive caffeine intake.
Clinical Significance: AF with RVR can lead to symptoms such as palpitations, fatigue, and shortness of breath. If left untreated, it can result in complications such as heart failure or stroke.
Multifocal Atrial Tachycardia (MAT)
Definition and Characteristics: Multifocal atrial tachycardia (MAT) is a type of tachycardia that arises from multiple ectopic foci within the atria. On an ECG, MAT is characterized by at least three distinct P wave morphologies, with a heart rate usually between 100 and 150 beats per minute. The rhythm is irregular, and the P-R intervals may vary.
Causes: MAT is often associated with chronic lung disease, particularly chronic obstructive pulmonary disease (COPD). It can also be triggered by electrolyte imbalances, drug toxicity, or heart failure.
Clinical Significance: MAT is often symptomatic, causing palpitations and dyspnea. It is important to treat the underlying cause, as this arrhythmia can be challenging to manage with antiarrhythmic medications alone.
Junctional Tachycardia
Definition and Characteristics: Junctional tachycardia arises from the atrioventricular (AV) junction, an area around the AV node. On an ECG, junctional tachycardia is characterized by a regular rhythm with a narrow QRS complex and a heart rate typically between 70 and 130 beats per minute. P waves may be inverted, absent, or occur after the QRS complex.
Causes: Junctional tachycardia can occur due to digitalis toxicity, ischemia, or post-cardiac surgery. It may also be idiopathic or related to congenital heart conditions.
Clinical Significance: Junctional tachycardia can be symptomatic, causing palpitations and dizziness. It may require treatment, particularly if it leads to hemodynamic instability.
Conclusion
Tachycardia encompasses a wide range of arrhythmias that can significantly impact a patient’s health. The ability to recognize and differentiate these types on an ECG is critical for appropriate management and treatment. From sinus tachycardia, which is often benign, to ventricular fibrillation, a life-threatening emergency, each type of tachycardia presents unique challenges in clinical practice. Early detection and accurate diagnosis can help guide effective treatment strategies, ultimately improving patient outcomes.