Heart failure and cardiac arrest are terms often used interchangeably, but they represent two distinct conditions with different causes, symptoms, and treatments. Both are serious heart-related conditions, but understanding their differences is crucial for proper diagnosis, treatment, and patient education. This article will delve into the differences between heart failure and cardiac arrest, exploring their definitions, causes, symptoms, treatment options, and outcomes.
Causes of Heart Failure
Heart failure can be caused by a variety of underlying conditions that damage or weaken the heart. Some of the most common causes include:
Coronary Artery Disease (CAD): A condition where the arteries that supply blood to the heart muscle become narrowed or blocked, leading to reduced blood flow and oxygen to the heart. This can result in heart muscle damage, contributing to heart failure.
Hypertension (High Blood Pressure): Chronic high blood pressure forces the heart to work harder to pump blood, which can eventually lead to the thickening and weakening of the heart muscle.
Myocardial Infarction (Heart Attack): When a part of the heart muscle is damaged due to a lack of blood supply, it can lead to a decrease in the heart’s pumping ability, contributing to heart failure.
Cardiomyopathy: A disease of the heart muscle that can be caused by genetic factors, infections, or other medical conditions.
Cardiomyopathy weakens the heart and can lead to heart failure.
Valvular Heart Disease: When the heart valves do not function properly, it can disrupt blood flow and strain the heart, leading to heart failure.
Diabetes: High blood sugar levels over time can damage blood vessels and the heart muscle, increasing the risk of heart failure.
SEE ALSO: The 5 Common Causes of Death from Heart Failure
Symptoms of Heart Failure
The symptoms of heart failure can vary depending on the severity of the condition and which side of the heart is affected.
Common symptoms include:
Shortness of Breath: Often occurring during physical activity or while lying down, shortness of breath is a hallmark symptom of heart failure.
Fatigue and Weakness: Reduced blood flow to the body’s organs and muscles can lead to persistent tiredness and a lack of energy.
Swelling (Edema): Fluid retention in the legs, ankles, feet, and abdomen is a common symptom of heart failure, often leading to significant discomfort.
Persistent Cough or Wheezing: Fluid buildup in the lungs can cause a chronic cough, wheezing, and difficulty breathing.
Rapid or Irregular Heartbeat: The heart may beat faster or irregularly as it tries to compensate for its decreased pumping ability.
Weight Gain: Sudden weight gain due to fluid retention is a common symptom of worsening heart failure.
Diagnosis And Treatment of Heart Failure
Diagnosing heart failure typically involves a combination of medical history, physical examination, and diagnostic tests such as echocardiography, electrocardiography (ECG), chest X-rays, and blood tests. These tests help determine the underlying cause and severity of heart failure.
Treatment for heart failure focuses on managing symptoms, slowing the progression of the disease, and improving quality of life. Common treatment options include:
Medications: Various medications are used to treat heart failure, including ACE inhibitors, beta-blockers, diuretics, and aldosterone antagonists. These drugs help lower blood pressure, reduce fluid buildup, and improve heart function.
Lifestyle Changes: Patients with heart failure are often advised to make lifestyle changes such as reducing salt intake, maintaining a healthy weight, quitting smoking, and engaging in regular physical activity.
Surgical Interventions: In some cases, surgical procedures such as coronary artery bypass grafting (CABG), valve repair or replacement, or implantation of a left ventricular assist device (LVAD) may be necessary to manage heart failure.
Heart Transplant: For patients with severe heart failure who do not respond to other treatments, a heart transplant may be considered.
Understanding Cardiac Arrest
Cardiac arrest is a sudden and often unexpected cessation of heart function, leading to a complete stoppage of blood flow to the brain and other vital organs. Unlike heart failure, which is a chronic condition, cardiac arrest is an acute and life-threatening emergency that requires immediate medical intervention.
Causes of Cardiac Arrest
Cardiac arrest can occur due to several underlying conditions, many of which are related to heart disease. Common causes include:
Ventricular Fibrillation (VF): A life-threatening arrhythmia where the heart’s ventricles quiver instead of contracting effectively, leading to a loss of blood flow. VF is the most common cause of cardiac arrest.
Ventricular Tachycardia (VT): A rapid heart rhythm that originates in the heart’s ventricles, which can lead to cardiac arrest if not treated promptly.
Severe Heart Attack: A large or severe heart attack can damage a significant portion of the heart muscle, leading to cardiac arrest.
Bradycardia: An abnormally slow heart rate can cause cardiac arrest if the heart cannot maintain adequate blood flow.
Electrolyte Imbalances: Abnormal levels of electrolytes such as potassium or magnesium can disrupt the heart’s electrical activity, leading to arrhythmias and cardiac arrest.
Drug Overdose or Poisoning: Certain drugs, including recreational drugs and medications, can cause cardiac arrest by disrupting the heart’s electrical system.
Respiratory Arrest: Severe respiratory failure, such as from choking, drowning, or suffocation, can lead to cardiac arrest due to a lack of oxygen.
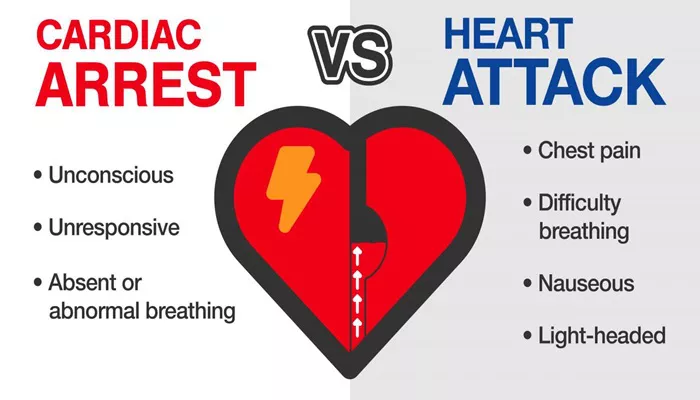
Symptoms of Cardiac Arrest
Cardiac arrest often occurs suddenly and without warning. The primary symptom is the sudden loss of consciousness and absence of a pulse.
Other symptoms that may precede cardiac arrest include:
Chest Pain or Discomfort: This may occur shortly before cardiac arrest, particularly if the arrest is related to a heart attack.
Shortness of Breath: Difficulty breathing or shortness of breath may precede cardiac arrest.
Dizziness or Lightheadedness: These symptoms may occur as the heart begins to fail.
Palpitations: The sensation of a racing or irregular heartbeat may precede cardiac arrest.
Diagnosis And Treatment of Cardiac Arrest
Cardiac arrest is diagnosed based on the absence of a pulse, unresponsiveness, and lack of breathing. Immediate treatment is essential to increase the chances of survival. Key components of treatment include:
Cardiopulmonary Resuscitation (CPR): CPR is a life-saving procedure that involves chest compressions and rescue breaths to maintain circulation and oxygenation until professional medical help arrives.
Defibrillation: A defibrillator is used to deliver an electric shock to the heart to restore a normal rhythm in cases of ventricular fibrillation or pulseless ventricular tachycardia.
Advanced Cardiac Life Support (ACLS): In a hospital or emergency setting, ACLS includes the use of medications, advanced airway management, and other interventions to treat the underlying cause of cardiac arrest.
Post-Resuscitation Care: After successful resuscitation, patients require intensive care to monitor and manage complications, prevent recurrence, and determine the underlying cause of the cardiac arrest.
Key Differences Between Heart Failure And Cardiac Arrest
Nature of the Condition:
Heart Failure: A chronic condition where the heart gradually loses its ability to pump blood effectively.
Cardiac Arrest: An acute emergency where the heart suddenly stops beating, leading to a complete loss of circulation.
Causes:
Heart Failure: Often caused by conditions that weaken or damage the heart over time, such as coronary artery disease, hypertension, and cardiomyopathy.
Cardiac Arrest: Typically caused by life-threatening arrhythmias like ventricular fibrillation or severe heart attacks.
Symptoms:
Heart Failure: Symptoms develop gradually and include shortness of breath, fatigue, swelling, and persistent cough.
Cardiac Arrest: Symptoms occur suddenly, with the most prominent being the sudden loss of consciousness and absence of a pulse.
Treatment:
Heart Failure: Managed with medications, lifestyle changes, and sometimes surgery or devices like LVADs.
Cardiac Arrest: Requires immediate CPR, defibrillation, and advanced cardiac life support.
Prognosis:
Heart Failure: Can be managed, allowing patients to live with the condition for many years, though it may progressively worsen.
Cardiac Arrest: Is often fatal without prompt intervention, with survival depending on immediate medical response.
Conclusion
While heart failure and cardiac arrest both involve the heart and can be life-threatening, they are fundamentally different conditions. Heart failure is a chronic disease characterized by the heart’s inability to pump blood effectively,leading to gradual symptoms and requiring ongoing management. Cardiac arrest is a sudden, acute event where the heart stops beating, necessitating immediate emergency treatment to prevent death.