Hyperlipidemia refers to an elevated level of lipids (fats) in the blood, including cholesterol and triglycerides, which are significant risk factors for cardiovascular disease. Borderline hyperlipidemia is a term used when lipid levels are higher than normal but not yet high enough to be classified as hyperlipidemia. This condition requires careful monitoring and lifestyle adjustments to prevent progression to full-blown hyperlipidemia and its associated health risks.
Understanding Lipid Levels And Their Importance
Lipids are essential components of our body, serving as building blocks for cell membranes, hormones, and energy storage.
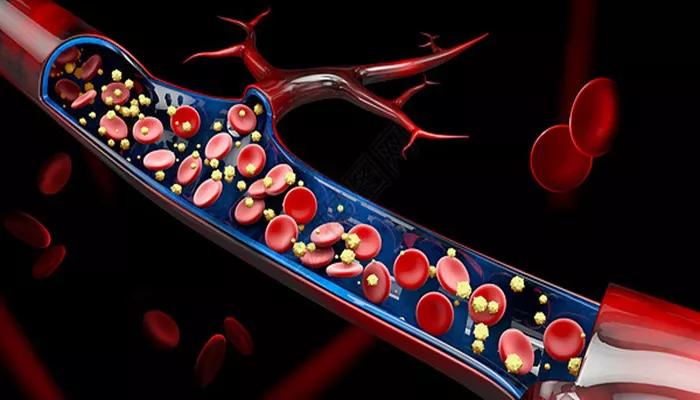
However, when lipid levels in the blood become imbalanced, they can contribute to the development of atherosclerosis, a condition characterized by the buildup of fatty deposits in the arterial walls. This can lead to narrowing and hardening of the arteries, increasing the risk of heart attack, stroke, and other cardiovascular diseases.
The Types of Lipids Involved
Cholesterol:
Low-Density Lipoprotein (LDL) Cholesterol: Often referred to as “bad” cholesterol, LDL cholesterol is responsible for transporting cholesterol from the liver to the rest of the body. High levels of LDL cholesterol can lead to plaque buildup in the arteries, increasing the risk of atherosclerosis.
High-Density Lipoprotein (HDL) Cholesterol: Known as “good” cholesterol, HDL cholesterol helps remove excess cholesterol from the bloodstream, transporting it back to the liver for excretion. Higher levels of HDL cholesterol are associated with a reduced risk of cardiovascular disease.
SEE ALSO: What Is Familial Combined Hyperlipidemia?
Triglycerides:
Triglycerides are a type of fat that serves as an energy source for the body. However, elevated levels of triglycerides are linked to an increased risk of atherosclerosis and pancreatitis.
Borderline Hyperlipidemia: Defining The Condition
The Thresholds of Borderline Hyperlipidemia
Borderline hyperlipidemia is identified through blood tests that measure lipid levels, including total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. The following ranges are commonly used to define borderline lipid levels:
Total Cholesterol: 200-239 mg/dL
LDL Cholesterol: 130-159 mg/dL
HDL Cholesterol: Less than 40 mg/dL (low) for men, less than 50 mg/dL (low) for women
Triglycerides: 150-199 mg/dL
Individuals with lipid levels within these ranges are considered to have borderline hyperlipidemia. While these levels are not high enough to warrant a diagnosis of hyperlipidemia, they indicate an increased risk for cardiovascular disease if left unmanaged.
Risk Factors for Developing Borderline Hyperlipidemia
Who is at Risk?
Several factors can contribute to the development of borderline hyperlipidemia, including:
Dietary Habits:
A diet high in saturated fats, trans fats, and cholesterol can elevate lipid levels in the blood. Consuming excessive amounts of red meat, full-fat dairy products, fried foods, and processed snacks increases the risk of borderline hyperlipidemia.
Sedentary Lifestyle:
Lack of physical activity contributes to weight gain and elevated lipid levels. Regular exercise helps increase HDL cholesterol levels and lower LDL cholesterol and triglycerides.
Genetics:
Family history plays a significant role in lipid levels. Individuals with a family history of hyperlipidemia or cardiovascular disease are at higher risk of developing borderline hyperlipidemia.
Obesity:
Being overweight or obese is closely associated with elevated lipid levels. Excess body fat, particularly around the abdomen, increases LDL cholesterol and triglyceride levels while decreasing HDL cholesterol.
Age and Gender:
Lipid levels tend to increase with age, particularly after menopause in women. Men are also at a higher risk of developing borderline hyperlipidemia at a younger age compared to women.
Medical Conditions:
Certain medical conditions, such as diabetes, hypothyroidism, and kidney disease, can contribute to abnormal lipid levels.
These conditions often require careful management to prevent the progression of borderline hyperlipidemia.
Smoking and Alcohol Consumption:
Smoking lowers HDL cholesterol levels and contributes to the buildup of plaque in the arteries. Excessive alcohol consumption can raise triglyceride levels and lead to liver damage, further increasing the risk of borderline hyperlipidemia.
The Health Implications of Borderline Hyperlipidemia
Potential Risks and Consequences
While borderline hyperlipidemia may not immediately lead to severe health issues, it is a significant warning sign that should not be ignored. The condition can progress to full-blown hyperlipidemia if left unmanaged, increasing the risk of the following complications:
Atherosclerosis:
As lipid levels rise, the risk of atherosclerosis increases. Plaque buildup in the arteries can lead to narrowed and hardened arteries, reducing blood flow to vital organs. This condition is a leading cause of heart attacks, strokes, and peripheral artery disease.
Cardiovascular Disease:
Borderline hyperlipidemia is a precursor to cardiovascular disease. Elevated LDL cholesterol and triglyceride levels, combined with low HDL cholesterol, contribute to the development of coronary artery disease, heart failure, and arrhythmias.
Pancreatitis:
High triglyceride levels associated with borderline hyperlipidemia can increase the risk of pancreatitis, a condition characterized by inflammation of the pancreas. Pancreatitis can cause severe abdominal pain, digestive issues, and, in some cases, life-threatening complications.
Metabolic Syndrome:
Borderline hyperlipidemia is often associated with other risk factors that make up metabolic syndrome, including high blood pressure, insulin resistance, and central obesity. Metabolic syndrome significantly increases the risk of type 2 diabetes, heart disease, and stroke.
Diagnosing Borderline Hyperlipidemia
How is Borderline Hyperlipidemia Identified?
Diagnosing borderline hyperlipidemia involves a thorough assessment of lipid levels through blood tests. The following steps are typically taken to diagnose and monitor the condition:
Lipid Panel:
A lipid panel is a blood test that measures total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. The results are used to determine whether lipid levels fall within the borderline range.
Risk Assessment:
Healthcare providers consider additional factors, such as family history, age, gender, smoking status, and the presence of other medical conditions, to assess an individual’s overall risk for cardiovascular disease.
Monitoring:
Regular monitoring of lipid levels is essential for individuals with borderline hyperlipidemia. This allows healthcare providers to track changes in lipid levels over time and adjust treatment plans accordingly.
Conclusion
Borderline hyperlipidemia is a critical condition that signals an increased risk of cardiovascular disease. While it may not yet meet the criteria for hyperlipidemia, it should be taken seriously and managed proactively. Through lifestyle modifications, regular monitoring, and, when necessary, medication, individuals with borderline hyperlipidemia can significantly reduce their risk of developing more severe health issues. By taking action early and making informed choices, it is possible to maintain healthy lipid levels and protect long-term heart health.