Atropine is a medication that has been widely used in medical practice, particularly in cardiology, for its powerful effects on the heart’s electrical system. It is an essential drug in the management of various types of arrhythmias, especially those related to the heart’s rhythm and rate. Understanding the role of atropine in treating arrhythmias can be crucial for both medical professionals and patients. This article delves into the specific arrhythmias that atropine is used to treat, how it works, and the scenarios where its application is most effective.
Understanding Arrhythmias And The Role of Atropine
Arrhythmias are disorders of the heart’s rhythm, where the heart may beat too fast, too slow, or irregularly. These conditions can range from benign to life-threatening, requiring different treatment strategies. Atropine is a key medication in managing certain arrhythmias, particularly those associated with bradycardia or slow heart rates.
Atropine works by blocking the action of the vagus nerve on the heart. The vagus nerve plays a significant role in controlling the heart’s rate by releasing acetylcholine, which slows down the heart rate. By inhibiting this effect, atropine increases the heart rate, making it an effective treatment for specific types of bradyarrhythmias.
Types of Arrhythmias Treated by Atropine
1. Sinus Bradycardia
Sinus bradycardia is one of the most common arrhythmias treated with atropine. In sinus bradycardia, the heart rate is slower than normal due to a decrease in the rate at which the sinus node, the heart’s natural pacemaker, generates electrical impulses. This can lead to symptoms such as dizziness, fatigue, shortness of breath, or even syncope (fainting).
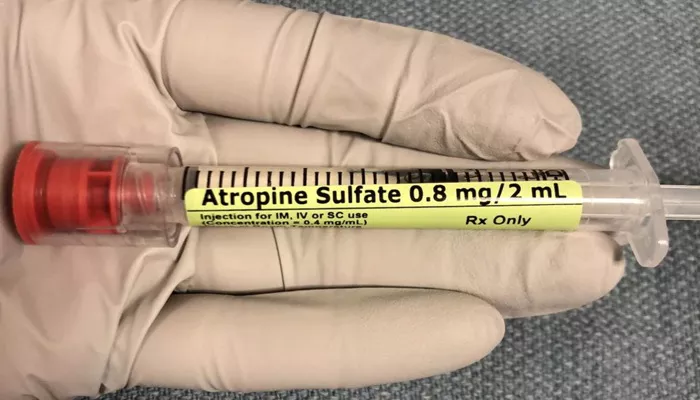
Atropine is particularly useful in acute settings where sinus bradycardia leads to symptomatic hypotension or compromised cardiac output. By blocking the parasympathetic influences on the heart, atropine increases the heart rate and improves hemodynamic stability. It is administered intravenously, and the effects are usually rapid, making it a first-line treatment in emergency situations.
SEE ALSO: What Are The Treatments for Atrial Arrhythmia?
2. Atrioventricular (AV) Block
Atrioventricular block refers to a condition where the conduction of electrical impulses from the atria to the ventricles is impaired. AV blocks are classified into three degrees, with second-degree and third-degree (complete heart block) being the most serious.
Atropine is primarily used in the management of second-degree AV block type I (Wenckebach block) and in some cases of third-degree AV block where the block occurs at the level of the AV node. In these conditions, the heart’s electrical signals are delayed or intermittently blocked, causing a slow ventricular rate. Atropine can help by increasing the conduction through the AV node, thereby improving the heart rate and symptoms associated with the block.
3. Junctional Escape Rhythm
Junctional escape rhythm is another arrhythmia where atropine is employed. This rhythm occurs when the primary pacemaker of the heart (the sinus node) fails, and the AV node takes over as the pacemaker, resulting in a slower heart rate.
In cases where junctional escape rhythm is symptomatic and leads to bradycardia, atropine can be effective in increasing the heart rate. By inhibiting vagal activity, atropine allows the sinus node to regain control or increases the intrinsic rate of the AV node, thus improving cardiac output.
Mechanism of Action of Atropine in Arrhythmias
Atropine is an anticholinergic agent that works by competitively inhibiting the action of acetylcholine on muscarinic receptors. In the context of arrhythmias, its primary effect is on the heart’s muscarinic receptors, which are part of the parasympathetic nervous system. By blocking these receptors, atropine reduces vagal tone on the heart, leading to an increase in the firing rate of the sinoatrial (SA) node and improved conduction through the AV node.
This action makes atropine particularly effective in treating bradyarrhythmias, where an abnormally slow heart rate compromises the circulation of blood and oxygen to vital organs.
Clinical Application of Atropine in Cardiology
1. Emergency Situations
In emergency settings, atropine is a critical drug used to manage symptomatic bradycardia. The American Heart Association (AHA) includes atropine in its Advanced Cardiovascular Life Support (ACLS) protocols as the first-line treatment for bradycardia with signs of poor perfusion.
For instance, in the case of a patient with acute myocardial infarction who develops sinus bradycardia, atropine can be administered to prevent further deterioration of cardiac output. The standard dose of atropine in such scenarios is 0.5 mg IV, which can be repeated every 3-5 minutes to a maximum of 3 mg.
2. Perioperative Bradycardia
Atropine is also used prophylactically to prevent bradycardia during surgery, particularly during procedures that involve anesthesia, which can enhance vagal tone. Anesthesia-induced bradycardia can lead to significant hypotension, and atropine is administered to counteract this effect and maintain stable hemodynamics.
3. Diagnostic Testing
In some diagnostic tests, such as the carotid sinus massage or tilt-table testing, atropine may be used to treat induced bradycardia or assist in the differentiation of various types of syncope. It helps by counteracting the excessive vagal stimulation that these tests may provoke.
Limitations And Considerations
1. Ineffectiveness in Certain Arrhythmias
While atropine is effective in treating various bradyarrhythmias, it is not useful for all types of arrhythmias. For instance, it is generally ineffective in treating arrhythmias like ventricular tachycardia or atrial fibrillation, where the underlying problem is not related to increased vagal tone.
2. Potential Side Effects
Atropine can have several side effects, particularly when used in higher doses. These include dry mouth, blurred vision, urinary retention, constipation, and in some cases, paradoxical bradycardia. Additionally, patients with glaucoma should avoid atropine as it can increase intraocular pressure.
3. Caution in Myocardial Infarction
In the context of myocardial infarction, while atropine can be beneficial in treating bradycardia, it must be used cautiously.
Excessive increase in heart rate can increase myocardial oxygen demand, potentially worsening ischemia. Therefore, careful monitoring is essential when administering atropine in patients with acute coronary syndromes.
Conclusion
Atropine is a valuable medication in the treatment of certain arrhythmias, particularly those associated with bradycardia. It is most effective in conditions such as sinus bradycardia, AV block, and junctional escape rhythm, where it works by increasing the heart rate and improving conduction through the AV node. Despite its widespread use, it is important to understand its limitations and potential side effects, particularly in patients with complex cardiovascular conditions. When used appropriately, atropine can be a life-saving drug in the management of arrhythmias, particularly in emergency and perioperative settings. In summary, atropine’s role in treating arrhythmias highlights its importance in modern cardiology, offering a quick and effective solution for bradyarrhythmias, ensuring better outcomes for patients with compromised heart rhythms.