Blood pressure regulation is a complex physiological process influenced by various factors, including the autonomic nervous system (ANS). Among the components of the ANS, the vagus nerve plays a critical role in controlling heart rate and blood pressure. This article explores how the vagus nerve can trigger a sudden drop in blood pressure, the mechanisms involved, and the clinical implications of this phenomenon.
The vagus nerve, the longest cranial nerve in the body, is a key component of the parasympathetic nervous system. It extends from the brainstem to various organs, including the heart, lungs, and digestive tract, and is instrumental in regulating heart rate and blood pressure.
The Vagus Nerve: Anatomy And Function
The vagus nerve, also known as cranial nerve X, originates in the medulla oblongata of the brainstem. It has a complex branching structure that innervates multiple organs throughout the body. The vagus nerve is responsible for several functions, including:
Heart Rate Regulation: The vagus nerve releases acetylcholine, a neurotransmitter that slows down the heart rate by acting on the heart’s pacemaker cells.
Gastrointestinal Function: It stimulates digestive processes by promoting peristalsis and the secretion of digestive enzymes.
Respiratory Function: The vagus nerve helps regulate breathing patterns and airway resistance.
Inflammatory Response: It plays a role in modulating the immune response and reducing inflammation.
SEE ALSO: Why Is Low Blood Pressure Bad for You?
Mechanisms of Blood Pressure Regulation by The Vagus Nerve
The vagus nerve influences blood pressure through several mechanisms:
1. Heart Rate Control
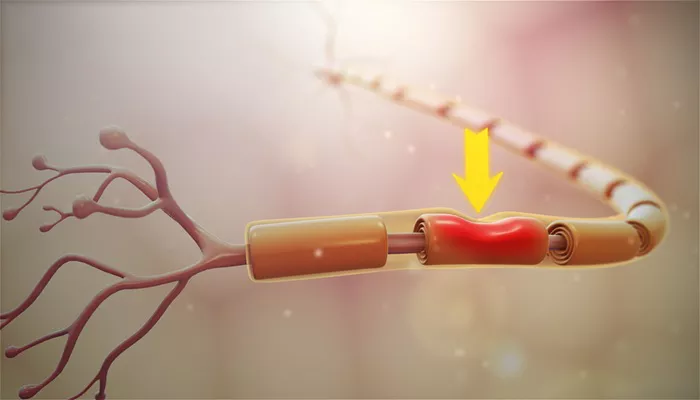
The vagus nerve exerts a direct effect on the heart by decreasing heart rate. When the vagus nerve is activated, it releases acetylcholine, which binds to muscarinic receptors in the heart. This action leads to a decrease in heart rate (negative chronotropic effect) and a reduction in the force of cardiac contractions (negative inotropic effect). As heart rate decreases, cardiac output also declines, which can lead to a drop in blood pressure.
2. Vasodilation
The vagus nerve can induce vasodilation, or the widening of blood vessels, through several pathways. When the vagus nerve is stimulated, it can release neurotransmitters that cause the smooth muscle in blood vessel walls to relax. This relaxation reduces vascular resistance, allowing blood to flow more easily and resulting in lower blood pressure.
3. Reflex Mechanisms
The vagus nerve is involved in several reflex mechanisms that can affect blood pressure. One notable example is the baroreceptor reflex, which helps maintain blood pressure homeostasis. Baroreceptors are specialized sensors located in the walls of blood vessels, particularly in the carotid arteries and aorta. When blood pressure rises, baroreceptors send signals to the brain, which in turn activates the vagus nerve to lower heart rate and induce vasodilation, ultimately reducing blood pressure.
Conversely, if blood pressure drops, the sympathetic nervous system is activated to increase heart rate and constrict blood vessels, raising blood pressure.
Vasovagal Syncope: A Clinical Example
One of the most common clinical scenarios in which the vagus nerve triggers a sudden drop in blood pressure is vasovagal syncope. This condition, also known as neurocardiogenic syncope, occurs when the body overreacts to certain triggers, leading to a sudden drop in heart rate and blood pressure, resulting in fainting.
Triggers of Vasovagal Syncope
Vasovagal syncope can be triggered by various factors, including:
Emotional Stress: Situations involving fear, anxiety, or distress can provoke a vasovagal response.
Pain or Injury: Experiencing severe pain or injury can stimulate the vagus nerve, leading to a drop in blood pressure.
Prolonged Standing: Standing for extended periods can cause blood to pool in the lower extremities, reducing blood flow to the brain and triggering a vasovagal response.
Heat Exposure: High temperatures can cause blood vessels to dilate, leading to a drop in blood pressure.
Dehydration: Low blood volume due to dehydration can exacerbate the effects of vasovagal syncope.
Pathophysiology of Vasovagal Syncope
During a vasovagal episode, the following physiological changes occur:
Increased Vagal Tone: The vagus nerve becomes overly active, leading to a significant decrease in heart rate (bradycardia).
Vasodilation: Blood vessels dilate, causing a drop in vascular resistance.
Reduced Cardiac Output: The combination of bradycardia and vasodilation leads to decreased cardiac output, resulting in insufficient blood flow to the brain.
Loss of Consciousness: The brain’s oxygen supply is compromised, leading to fainting.
Diagnosis of Vasovagal Syncope
Diagnosing vasovagal syncope typically involves a thorough medical history and physical examination. Healthcare providers may also conduct tests to rule out other potential causes of syncope, such as cardiac arrhythmias or neurological disorders. Common diagnostic tests include:
Electrocardiogram (ECG): This test measures the electrical activity of the heart and can identify arrhythmias.
Tilt Table Test: This test assesses how the body responds to changes in position and can help provoke a vasovagal response in a controlled setting.
Holter Monitor: A portable ECG monitor worn for 24-48 hours to capture heart rhythm abnormalities.
Treatment And Management of Vasovagal Syncope
While vasovagal syncope is generally not dangerous, it can lead to injuries from falls. Management strategies may include:
Lifestyle Modifications: Individuals may be advised to avoid known triggers, such as prolonged standing or sudden changes in position.
Physical Counterpressure Maneuvers: Techniques such as leg crossing or tensing the leg muscles can help increase venous return and prevent fainting.
Medications: In some cases, medications such as fludrocortisone or midodrine may be prescribed to help increase blood volume and blood pressure.
Education: Patients should be educated about the condition and how to recognize early symptoms to prevent fainting.
Conclusion
The vagus nerve plays a pivotal role in regulating blood pressure through its influence on heart rate and vascular tone.
When the vagus nerve is overstimulated, it can trigger a sudden drop in blood pressure, leading to conditions such as vasovagal syncope. Understanding the mechanisms by which the vagus nerve affects blood pressure is crucial for diagnosing and managing conditions associated with syncope and other cardiovascular issues.
Healthcare providers should be aware of the signs and symptoms of vagal nerve dysfunction and consider the vagus nerve’s role in blood pressure regulation when evaluating patients with unexplained syncope or dizziness. Through appropriate diagnosis and management strategies, individuals can effectively mitigate the risks associated with sudden drops in blood pressure and improve their overall quality of life.