Coronary artery disease (CAD) remains one of the leading causes of morbidity and mortality worldwide. A critical marker for CAD is the presence of coronary calcium buildup, which reflects the extent of calcification within the coronary arteries. This buildup is not merely a byproduct of aging but rather a complex process influenced by various factors, many of which are modifiable through lifestyle changes and medical interventions. Understanding the cause of coronary calcium buildup is essential for prevention and management, helping to reduce the burden of heart disease.
What Is Coronary Calcium Buildup?
Coronary calcium buildup refers to the accumulation of calcium deposits in the coronary arteries, the vessels responsible for supplying oxygen-rich blood to the heart muscle. These calcium deposits are part of the broader process of atherosclerosis, where plaques made up of fats, cholesterol, calcium, and other substances build up in the walls of arteries.
Over time, these plaques harden and narrow the arteries, reducing blood flow to the heart and increasing the risk of heart attack and other cardiovascular events.
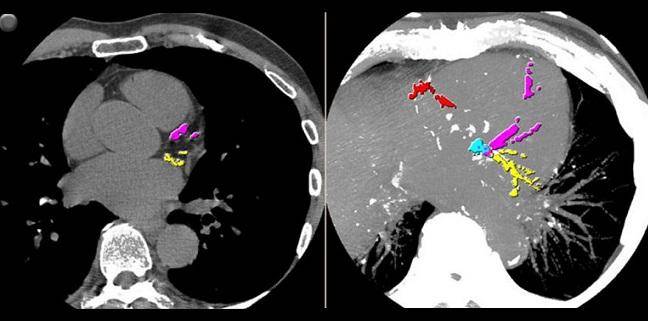
The degree of coronary calcium buildup can be assessed through a coronary artery calcium (CAC) score, which is measured using a specialized CT scan. A higher CAC score indicates more extensive calcium deposits, correlating with a greater risk of coronary artery disease.
The Role of Atherosclerosis in Coronary Calcium Buildup
Atherosclerosis is the primary process underlying coronary calcium buildup. It begins with damage to the inner lining of the arteries, known as the endothelium. This damage can result from various factors, including high blood pressure, smoking, diabetes, high cholesterol levels, and chronic inflammation.
Once the endothelium is damaged, it becomes more permeable to lipids, particularly low-density lipoprotein (LDL) cholesterol. These lipids penetrate the arterial wall and undergo oxidation, triggering an inflammatory response. Immune cells, including macrophages, are recruited to the site of injury, where they engulf the oxidized LDL, transforming into foam cells. The accumulation of these foam cells contributes to the formation of a fatty streak, the earliest visible sign of atherosclerosis.
As the process progresses, the fatty streak evolves into a more complex plaque. Smooth muscle cells migrate from the middle layer of the artery to the intima (the inner layer), where they proliferate and secrete extracellular matrix proteins, further stabilizing the plaque. Over time, calcium deposits form within the plaque, contributing to the hardening of the arteries.
The calcification process is thought to be a defensive mechanism by the body to stabilize the atherosclerotic plaque, making it less likely to rupture. However, while calcified plaques are less prone to rupture compared to soft plaques, their presence still indicates significant underlying atherosclerosis and an increased risk of cardiovascular events.
Key Factors Contributing to Coronary Calcium Buildup
1. High Cholesterol Levels
One of the most well-established risk factors for coronary calcium buildup is elevated cholesterol levels, particularly LDL cholesterol. LDL cholesterol plays a central role in the development of atherosclerosis by depositing in the arterial walls and undergoing oxidation. The oxidized LDL is then taken up by macrophages, leading to the formation of foam cells and contributing to plaque development.
Conversely, high-density lipoprotein (HDL) cholesterol, often referred to as “good” cholesterol, helps remove cholesterol from the arteries and transport it back to the liver for excretion. Low levels of HDL cholesterol are associated with an increased risk of coronary calcium buildup and subsequent cardiovascular disease.
2. Hypertension (High Blood Pressure)
Hypertension is another significant risk factor for coronary calcium buildup. Chronic high blood pressure exerts excessive force on the arterial walls, leading to endothelial damage. This damage promotes the infiltration of lipids into the arterial wall, accelerating the atherosclerotic process.
Moreover, hypertension contributes to vascular remodeling, where the structure of blood vessels changes in response to sustained high pressure. This remodeling often involves increased calcification of the arterial wall, further contributing to coronary calcium buildup.
3. Smoking
Smoking is a well-known risk factor for cardiovascular disease and is closely linked to the development of atherosclerosis and coronary calcium buildup. The chemicals in tobacco smoke cause direct damage to the endothelium, promoting inflammation and oxidative stress. These factors accelerate the atherosclerotic process, leading to the formation and calcification of plaques in the coronary arteries.
Additionally, smoking reduces HDL cholesterol levels and increases the likelihood of plaque rupture, which can result in a heart attack or stroke.
4. Diabetes Mellitus
Diabetes is a major contributor to coronary artery disease and is strongly associated with an increased risk of coronary calcium buildup. High blood glucose levels in diabetes lead to the formation of advanced glycation end-products (AGEs), which contribute to endothelial dysfunction and promote inflammation and oxidative stress in the arterial wall.
Moreover, diabetes is often accompanied by other metabolic abnormalities, such as dyslipidemia (abnormal cholesterol levels) and hypertension, which further exacerbate the atherosclerotic process and contribute to calcium deposition in the coronary arteries.
SEE ALSO: How Long Can You Live with Unstable Angina?
5. Chronic Inflammation
Inflammation plays a central role in the development and progression of atherosclerosis. Chronic low-grade inflammation, often driven by factors such as obesity, metabolic syndrome, and autoimmune diseases, can lead to persistent endothelial dysfunction and promote the deposition of calcium in the arterial walls.
Markers of inflammation, such as C-reactive protein (CRP), are often elevated in individuals with atherosclerosis and are associated with an increased risk of coronary artery disease. These inflammatory processes contribute to the formation and calcification of atherosclerotic plaques, increasing the burden of coronary calcium buildup.
6. Age and Gender
Age is one of the most significant non-modifiable risk factors for coronary calcium buildup. As individuals age, the cumulative exposure to risk factors such as high cholesterol, hypertension, and inflammation leads to an increased likelihood of atherosclerosis and coronary calcium deposition. The process of vascular calcification is accelerated with aging, making older adults more susceptible to coronary artery disease.
Gender also plays a role, with men typically experiencing coronary calcium buildup at an earlier age compared to women.
However, postmenopausal women are at increased risk due to the loss of protective effects from estrogen, which helps maintain vascular health.
7. Genetic Factors
Genetic predisposition plays a role in the development of coronary calcium buildup. Individuals with a family history of coronary artery disease are more likely to develop atherosclerosis and experience calcium deposition in the coronary arteries. Specific genetic variations related to lipid metabolism, inflammation, and calcium regulation may contribute to an increased risk of coronary calcium buildup.
8. Dietary Factors
Dietary habits significantly influence the risk of coronary calcium buildup. Diets high in saturated fats, trans fats, and cholesterol can lead to elevated LDL cholesterol levels, promoting the development of atherosclerosis and calcification of the arteries.
Conversely, diets rich in fruits, vegetables, whole grains, and healthy fats, such as those found in the Mediterranean diet, have been shown to reduce the risk of coronary artery disease. These diets are associated with lower levels of inflammation, improved lipid profiles, and reduced oxidative stress, all of which contribute to a lower burden of coronary calcium buildup.
9. Physical Inactivity
Physical inactivity is a well-recognized risk factor for coronary artery disease and coronary calcium buildup. Regular physical activity helps maintain a healthy weight, improves lipid profiles, lowers blood pressure, and reduces inflammation, all of which contribute to the prevention of atherosclerosis and vascular calcification.
Sedentary behavior, on the other hand, is associated with an increased risk of obesity, diabetes, and hypertension, all of which are linked to coronary calcium buildup.
Prevention And Management of Coronary Calcium Buildup
Preventing and managing coronary calcium buildup involves addressing the underlying risk factors for atherosclerosis.
Lifestyle modifications, such as adopting a heart-healthy diet, engaging in regular physical activity, quitting smoking, and managing stress, are foundational to reducing the risk of coronary calcium buildup.
In addition to lifestyle changes, pharmacological interventions may be necessary to control risk factors such as high cholesterol, hypertension, and diabetes. Statins, for example, are commonly prescribed to lower LDL cholesterol levels and reduce the progression of atherosclerosis. Anti-hypertensive medications help control blood pressure, while medications for diabetes help regulate blood glucose levels and reduce the risk of vascular complications.
For individuals with a high CAC score or significant coronary calcium buildup, more aggressive interventions may be warranted, such as the use of antiplatelet therapy, coronary revascularization, or other procedures to improve blood flow to the heart.
Conclusion
Coronary calcium buildup is a key marker of atherosclerosis and an important predictor of cardiovascular risk. The causes of coronary calcium buildup are multifactorial, involving a combination of genetic, environmental, and lifestyle factors.
Understanding these causes is essential for preventing and managing coronary artery disease, ultimately reducing the burden of heart disease and improving cardiovascular health. By addressing the underlying risk factors and implementing appropriate interventions, it is possible to slow the progression of coronary calcium buildup and reduce the risk of life-threatening cardiovascular events.