Coronary artery disease (CAD) is a leading cause of morbidity and mortality worldwide. It occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to a buildup of fatty deposits, known as plaques. This condition can lead to chest pain (angina), heart attacks, and other serious complications. To diagnose and treat CAD effectively, two important medical procedures are commonly used: coronary angiography and percutaneous coronary intervention (PCI). While these procedures are related, they serve different purposes and are performed in distinct ways. This article will explore the differences between coronary angiography and PCI, their indications, procedures, risks, and benefits.
Understanding Coronary Angiography
Coronary angiography is a specialized imaging technique used to visualize the coronary arteries. It is often referred to as a coronary angiogram. This procedure helps determine the presence and severity of blockages or narrowings in the coronary arteries.
Purpose of Coronary Angiography
The primary purpose of coronary angiography is to diagnose coronary artery disease. It provides critical information about the condition of the coronary arteries, helping healthcare providers assess the extent of any blockage and plan appropriate treatment.
How Coronary Angiography Works
Coronary angiography is performed in a specialized area called a catheterization lab. The procedure typically involves the following steps:
Preparation: The patient is usually asked to fast for several hours before the procedure. An intravenous (IV) line is placed to administer medications and fluids.
Accessing the Artery: A local anesthetic is applied to the access site, usually in the wrist (radial artery) or groin (femoral artery). A small incision is made, and a sheath is inserted into the artery.
Inserting the Catheter: A thin, flexible tube called a catheter is threaded through the sheath and guided to the coronary arteries. This is monitored using real-time X-ray imaging.
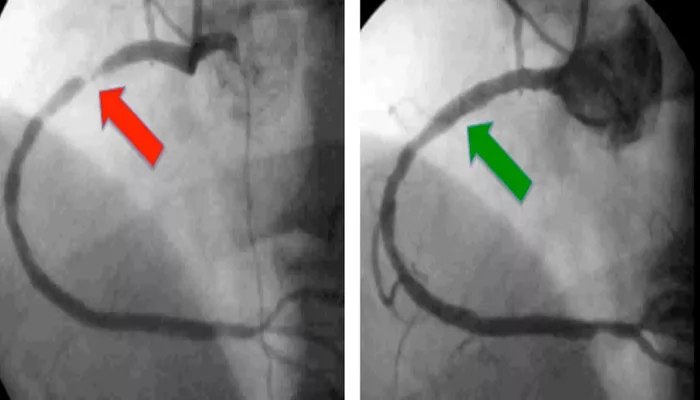
Injecting Contrast Dye: Once the catheter is in place, a contrast dye is injected through the catheter into the coronary arteries. This dye makes the arteries visible on X-ray images.
Taking Images: A series of X-ray images are taken to visualize the coronary arteries. These images help identify any blockages or narrowings.
Assessment and Recovery: After the images are captured, the catheter is removed, and pressure is applied to the access site to prevent bleeding. The patient is monitored for a short period before being discharged.
SEE ALSO: What Are 5 Symptoms of Coronary Artery Disease
Understanding Percutaneous Coronary Intervention (PCI)
Percutaneous coronary intervention, commonly known as PCI, is a minimally invasive procedure used to treat narrowed or blocked coronary arteries. It is often performed immediately after coronary angiography if significant blockages are identified.
Purpose of PCI
The primary goal of PCI is to restore blood flow to the heart muscle by opening narrowed or blocked arteries. This is particularly important in patients experiencing angina or those who have suffered a heart attack.
How PCI Works
The PCI procedure typically follows the same initial steps as coronary angiography. However, if significant blockages are found, additional steps are taken to treat them:
Balloon Angioplasty: Once the catheter is in place and the blockage is identified, a small balloon attached to the catheter is inflated at the site of the narrowing. This process compresses the plaque against the artery walls, widening the artery and improving blood flow.
Stent Placement: In most cases, a stent—a small mesh tube made of metal—is placed in the artery to keep it open after the balloon is deflated and removed. The stent helps prevent the artery from narrowing again.
Monitoring and Recovery: After the procedure, the patient is monitored for any complications. They may need to stay in the hospital for a short period, especially if a stent was placed.
Key Differences Between Coronary Angiography And PCI
While coronary angiography and PCI are often performed together, they serve different purposes and have distinct characteristics:
Purpose:
Coronary Angiography: Primarily a diagnostic procedure to visualize coronary arteries and assess the presence and severity of blockages.
PCI: A therapeutic procedure aimed at treating narrowed or blocked arteries to restore blood flow to the heart.
Procedure:
Coronary Angiography: Involves the injection of contrast dye and imaging of the coronary arteries without any intervention.
PCI: Involves balloon angioplasty and stent placement to treat identified blockages.
Outcome:
Coronary Angiography: Provides information to guide further treatment but does not directly treat the condition.
PCI: Actively treats coronary artery disease by improving blood flow and relieving symptoms.
Indications for Each Procedure
Both coronary angiography and PCI are indicated under specific circumstances:
Coronary Angiography:
Patients with symptoms of angina or chest pain.
Individuals with risk factors for coronary artery disease, such as diabetes, hypertension, or a family history of heart disease.
Patients requiring assessment of coronary artery disease before surgery or other interventions.
PCI:
Patients with significant coronary artery blockages identified during angiography.
Individuals experiencing acute coronary syndromes, such as ST-elevation myocardial infarction (STEMI) or unstable angina.
Patients with chronic stable angina who do not respond to medical therapy.
Risks And Complications
Both coronary angiography and PCI are generally safe procedures, but they do carry some risks:
Coronary Angiography:
Allergic reactions to contrast dye.
Bleeding or hematoma at the access site.
Infection at the catheter insertion site.
Rarely, complications such as heart attack or stroke.
PCI:
Risks associated with coronary angiography, plus:
Re-stenosis (narrowing of the artery again) at the stent site.
Blood clots forming on the stent.
Damage to the artery or surrounding structures.
Need for emergency bypass surgery in rare cases.
Conclusion
In summary, coronary angiography and percutaneous coronary intervention (PCI) are two essential procedures in the diagnosis and treatment of coronary artery disease. While coronary angiography serves as a diagnostic tool to visualize the coronary arteries, PCI is a therapeutic intervention aimed at treating identified blockages.
Understanding the differences between these procedures is crucial for patients and healthcare providers alike, as it helps inform treatment decisions and optimize patient outcomes.
Both procedures are generally safe and effective, offering significant benefits in managing coronary artery disease. By recognizing the indications, risks, and benefits of each procedure, patients can work closely with their healthcare team to make informed decisions about their cardiovascular health.’