Percutaneous coronary intervention (PCI) is a minimally invasive medical procedure used primarily to treat narrowing or blockage of the coronary arteries, which supply blood to the heart muscle. This condition, known as coronary artery disease (CAD), can lead to serious health issues such as angina (chest pain) and myocardial infarction (heart attack). PCI is a critical intervention that can alleviate symptoms, restore blood flow, and improve the quality of life for patients with heart disease.
What Is Coronary Artery Disease?
Coronary artery disease is one of the leading causes of morbidity and mortality worldwide. It occurs when the coronary arteries become narrowed or blocked due to the buildup of fatty deposits, known as plaque. This process is called atherosclerosis. As the plaque accumulates, it restricts blood flow to the heart muscle, which can lead to chest pain, shortness of breath, and other symptoms. In severe cases, a complete blockage can result in a heart attack, where a portion of the heart muscle is damaged due to lack of blood supply.
The Role of Percutaneous Coronary Intervention
PCI plays a vital role in the management of coronary artery disease. It is designed to open up narrowed or blocked arteries, restoring blood flow to the heart. Unlike traditional open-heart surgery, PCI is less invasive and typically involves a shorter recovery time. The procedure can be performed in a catheterization laboratory, often referred to as a “cath lab,” and usually takes about 30 minutes to 2 hours.
How Percutaneous Coronary Intervention Works
The PCI procedure involves several key steps:
Preparation: Before the procedure, the patient is typically given medications to help them relax. The area where the catheter will be inserted, usually the wrist or groin, is cleaned and sterilized.
Accessing the Artery: A small incision is made to access the femoral artery in the groin or the radial artery in the wrist. A sheath, which is a thin plastic tube, is inserted into the artery to provide access for the catheter.
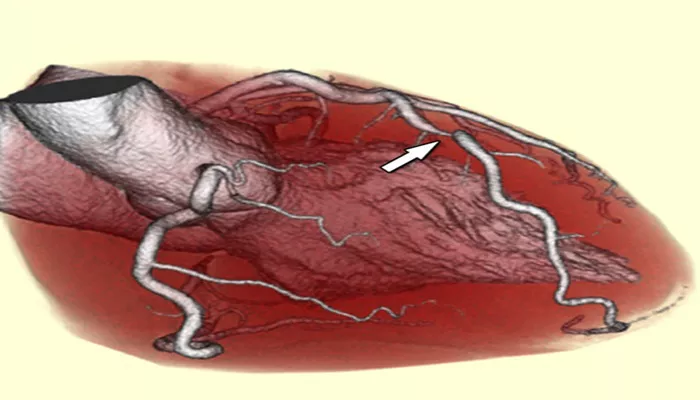
Guiding the Catheter: A catheter, which is a long, flexible tube, is threaded through the sheath and guided through the blood vessels to the coronary arteries. Fluoroscopy, a type of real-time X-ray imaging, is used to visualize the catheter’s position.
Injecting Contrast Dye: Once the catheter is in place, a contrast dye is injected through it into the coronary arteries. This dye helps to highlight the arteries on the X-ray images, allowing the cardiologist to identify the location and severity of any blockages.
Balloon Angioplasty: A second catheter equipped with a small balloon is then advanced to the narrowed area of the artery.
The balloon is inflated, which compresses the plaque against the artery wall, widening the artery and restoring blood flow.
Stent Placement: In most cases, a stent—a small mesh tube—is placed in the artery during the procedure. The stent helps to keep the artery open and prevent it from narrowing again. Drug-eluting stents, which release medication to reduce the risk of restenosis (re-narrowing of the artery), are commonly used.
Completion: After the stent is placed, the balloon is deflated and removed along with the catheter. The sheath is also removed, and pressure is applied to the access site to prevent bleeding.
Recovery: Patients are usually monitored for a few hours after the procedure. Many can go home the same day or the next day, depending on their condition.
SEE ALSO: What Happens in Coronary Steal Syndrome?
Indications for Percutaneous Coronary Intervention
PCI is indicated for various conditions related to coronary artery disease, including:
Stable Angina: Patients with stable angina who experience chest pain during physical activity may benefit from PCI to relieve symptoms and improve exercise tolerance.
Unstable Angina: In cases of unstable angina, where chest pain occurs at rest or with minimal exertion, PCI can provide urgent relief and prevent heart attacks.
Acute Myocardial Infarction: PCI is often the preferred treatment for patients experiencing a heart attack, especially if performed promptly.
It can restore blood flow to the heart muscle and minimize damage.
High-Risk Stress Test Results: Patients with abnormal results from stress tests indicating significant coronary artery blockages may be candidates for PCI to improve blood flow.
Benefits of Percutaneous Coronary Intervention
The benefits of PCI are numerous, including:
Minimally Invasive: PCI is less invasive than traditional open-heart surgery, resulting in reduced pain, shorter recovery times, and fewer complications.
Immediate Relief: Many patients experience immediate relief from symptoms such as chest pain and shortness of breath following the procedure.
Improved Quality of Life: By restoring blood flow to the heart, PCI can significantly enhance a patient’s quality of life, allowing them to return to normal activities.
Reduced Risk of Heart Attack: For patients with significant blockages, PCI can lower the risk of future heart attacks by improving blood flow and reducing strain on the heart.
Risks And Complications of Percutaneous Coronary Intervention
While PCI is generally safe, it is not without risks. Potential complications include:
Bleeding: There is a risk of bleeding at the access site, particularly if the femoral artery is used.
Infection: As with any invasive procedure, there is a risk of infection at the catheter insertion site.
Allergic Reactions: Some patients may have allergic reactions to the contrast dye used during the procedure.
Blood Clots: There is a risk of blood clots forming in the stent, which can lead to blockage of the artery (stent thrombosis).
Heart Arrhythmias: Some patients may experience irregular heartbeats during or after the procedure.
Kidney Damage: The contrast dye used in PCI can potentially harm kidney function, particularly in patients with pre-existing kidney issues.
Post-Procedure Care And Lifestyle Changes
After undergoing PCI, patients will typically be advised on post-procedure care and lifestyle modifications to enhance heart health and prevent further cardiovascular issues. Key recommendations include:
Medications: Patients may be prescribed antiplatelet medications, such as aspirin or clopidogrel, to reduce the risk of blood clots. It is crucial to take these medications as directed.
Dietary Changes: A heart-healthy diet low in saturated fats, cholesterol, and sodium can help manage risk factors for coronary artery disease.
Regular Exercise: Engaging in regular physical activity can improve cardiovascular health. Patients should consult their healthcare provider for a safe exercise plan.
Smoking Cessation: Quitting smoking is one of the most effective ways to improve heart health and reduce the risk of future heart problems.
Conclusion
Percutaneous coronary intervention (PCI) is a vital procedure for treating coronary artery disease and restoring blood flow to the heart. By understanding the process, indications, benefits, and potential risks associated with PCI, patients can make informed decisions about their heart health. Early intervention through PCI can lead to significant improvements in symptoms and quality of life, ultimately reducing the risk of serious cardiovascular events.