Fetal arrhythmia is a condition where a fetus experiences an abnormal heart rhythm. This irregular heartbeat can either be too fast (tachycardia) or too slow (bradycardia), and it poses significant concerns for fetal well-being, particularly regarding oxygenation. Proper oxygenation is crucial for fetal development, as the growing fetus relies heavily on the oxygen-rich blood supplied through the placenta. In this article, we will explore the mechanisms by which fetal arrhythmia can affect fetal oxygenation, the types of fetal arrhythmia, and how clinicians manage these risks.
What Is Fetal Oxygenation?
Fetal oxygenation is the process through which oxygen is transferred from the mother to the fetus via the placenta and umbilical cord. Unlike postnatal oxygenation, where breathing supplies oxygen, the fetus depends entirely on the maternal blood supply. Oxygenated blood reaches the fetus through the umbilical vein, and the fetal circulation is structured to prioritize oxygen delivery to vital organs such as the brain, heart, and liver. The efficiency of oxygen transfer depends on factors such as placental function, maternal oxygen levels, and, crucially, the fetal heart’s ability to pump blood effectively.
How Fetal Heart Rhythm Impacts Oxygenation
The fetal heart is responsible for circulating blood, and any irregularities in its rhythm can directly influence the amount of oxygenated blood delivered to fetal tissues. Fetal arrhythmias disrupt the normal coordination between the chambers of the heart, affecting both the rate and volume of blood flow. When the heart rhythm becomes irregular, the pumping efficiency of the fetal heart may be compromised, potentially leading to poor tissue oxygenation and distress for the fetus.
SEE ALSO: Can Arrhythmia Cause Blood Clots?
Types of Fetal Arrhythmias And Their Effects on Oxygenation
Different types of fetal arrhythmias can affect oxygenation in varying ways. Some arrhythmias have a greater potential to compromise oxygen delivery, depending on the heart rate and rhythm disturbances. Below, we examine the most common types of fetal arrhythmia and their impact on fetal oxygenation.
1. Fetal Tachycardia
Fetal tachycardia is characterized by a heart rate exceeding 160 beats per minute (bpm). There are two primary forms of tachycardia: sinus tachycardia and supraventricular tachycardia (SVT).
Sinus Tachycardia: This form of tachycardia typically results from maternal or fetal stress, such as fever, dehydration, or infections. Sinus tachycardia may be less harmful than other forms, but sustained high heart rates can limit the filling time of the fetal heart, reducing cardiac output and oxygen delivery.
Supraventricular Tachycardia (SVT): This type of tachycardia is often more concerning, with rates reaching up to 300 bpm. SVT disrupts the synchronization of atrial and ventricular contractions, significantly affecting cardiac output. The rapid heart rate reduces the time available for the ventricles to fill with blood between contractions, leading to lower stroke volume. Consequently, the fetus may not receive adequate oxygenation, potentially leading to hypoxia.
2. Fetal Bradycardia
Fetal bradycardia is defined by a heart rate of fewer than 110 bpm. Prolonged bradycardia can severely impact fetal oxygenation.
Sinus Bradycardia: In some cases, sinus bradycardia may be benign, particularly if the cause is transient, such as maternal hypotension. However, prolonged or recurrent episodes of bradycardia can reduce cardiac output, limiting the delivery of oxygen-rich blood to fetal tissues.
Complete Heart Block (CHB): Also known as atrioventricular block, CHB is a more serious form of bradycardia in which the electrical signals between the atria and ventricles are blocked. In cases of CHB, the fetal heart rate may drop to as low as 50 bpm. The slow heart rate significantly decreases cardiac output and blood flow to critical organs, heightening the risk of fetal hypoxia and hydrops fetalis, a condition marked by severe swelling caused by fluid accumulation.
3. Irregular Fetal Heart Rhythms
In addition to tachycardia and bradycardia, some fetuses experience irregular heart rhythms that can still impact oxygenation, even if the heart rate remains within normal limits.
Premature Atrial Contractions (PACs): These are the most common form of fetal arrhythmia and are usually benign. PACs occur when an extra heartbeat originates from the atria, disrupting the normal rhythm.
Though PACs rarely impact fetal oxygenation, if frequent or sustained, they may evolve into more concerning forms of arrhythmia such as SVT.
Premature Ventricular Contractions (PVCs): PVCs occur when extra beats originate in the ventricles. While less common than PACs, frequent PVCs may cause inefficient cardiac contractions, especially if they lead to a more sustained arrhythmia.
Impact of Poor Oxygenation on Fetal Health
The oxygenation of the fetus is vital for normal growth and development. Oxygen deprivation, even for a short time, can lead to a range of complications, depending on the severity and duration of hypoxia. When fetal oxygenation is compromised due to arrhythmia, the following outcomes may occur:
Fetal Hypoxia: Hypoxia occurs when the fetus does not receive enough oxygen to meet its metabolic needs. It can lead to acidosis, organ damage, and developmental delays if not addressed. In severe cases, prolonged hypoxia can result in stillbirth.
Intrauterine Growth Restriction (IUGR): Inadequate oxygenation can stunt fetal growth, resulting in IUGR. Babies born with IUGR are at higher risk of complications, including respiratory distress, neurological impairment, and long-term developmental challenges.
Hydrops Fetalis: This is a severe form of fetal heart failure that occurs when fluid accumulates in multiple compartments of the fetus, including the lungs, abdomen, and skin. Arrhythmias like SVT or CHB are common causes of hydrops fetalis due to their effects on oxygenation and cardiac output. Hydrops fetalis can be life-threatening if not treated promptly.
Monitoring And Management of Fetal Arrhythmia
The management of fetal arrhythmia is essential to minimizing its impact on oxygenation. Early detection and monitoring of arrhythmia allow clinicians to intervene before significant complications develop.
1. Prenatal Monitoring
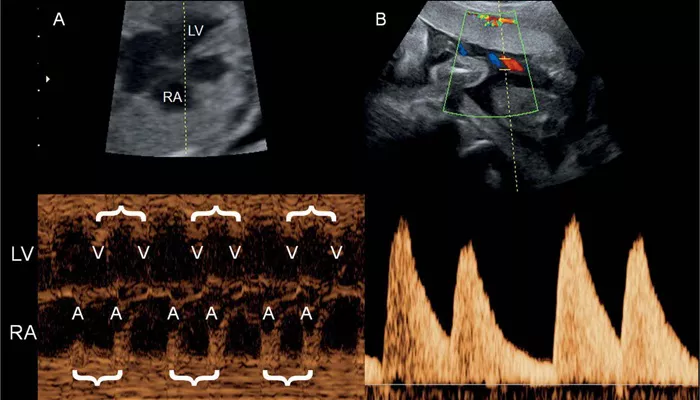
Routine fetal monitoring, particularly through ultrasound and Doppler studies, helps identify abnormal heart rhythms.
Fetal echocardiography is often used to assess the structure and function of the fetal heart in cases of arrhythmia.
Heart Rate Monitoring: During pregnancy, fetal heart rate is routinely checked to ensure it remains within the normal range. Any deviation from the normal rhythm may prompt further investigation.
Fetal Doppler Ultrasound: Doppler ultrasound measures blood flow through the umbilical artery and fetal vessels, providing insight into how well oxygenated blood is reaching the fetus.
2. Treatment Options
Depending on the type and severity of the arrhythmia, several treatment options may be considered.
Medications: In some cases, medications may be given to the mother to correct the fetal arrhythmia. For example, anti-arrhythmic drugs like digoxin or sotalol are used to treat SVT. These medications can cross the placenta and stabilize the fetal heart rhythm.
Delivery: If the arrhythmia poses an immediate risk to the fetus, early delivery may be considered. In cases of hydrops fetalis or sustained bradycardia, prompt delivery allows the medical team to address oxygenation issues and provide life-saving interventions.
Conclusion
Fetal arrhythmia can significantly affect fetal oxygenation, depending on the type and severity of the arrhythmia.
Tachycardia, bradycardia, and irregular heart rhythms can compromise the fetal heart’s ability to deliver oxygenated blood to vital organs. Effective prenatal monitoring and timely intervention are crucial to preventing complications such as fetal hypoxia, IUGR, and hydrops fetalis.
Related topics:
- Why Do I Get Arrhythmia After Eating?
- What Is Sinus Arrhythmia on An Ecg?
- What Is The Clinical Significance of an Arrhythmia?