Autologous coronary artery atherosclerosis refers to the formation of plaque within the arteries of the heart that originates from the body’s own cells and materials. This process is part of a broader condition called atherosclerosis, which is the hardening and narrowing of the arteries due to the buildup of fatty deposits (plaque). When this occurs in the coronary arteries, which supply blood to the heart muscle, it can lead to serious cardiovascular problems, such as heart attacks, angina, and heart failure.
What Is Autologous in Atherosclerosis?
The term “autologous” refers to something that originates from the individual’s own body. In the context of autologous coronary artery atherosclerosis, it describes how the plaque material in the coronary arteries consists of substances produced by the body, such as cholesterol and other lipids, immune cells, and smooth muscle cells. This type of plaque formation is a result of internal, rather than external, factors.
Unlike conditions like infections, where foreign agents are involved, the plaques in autologous coronary artery atherosclerosis are composed of the body’s own cells and metabolic products. This makes it an internal process driven by various factors such as:
- Genetics
- Diet
- Lifestyle choices
- Chronic inflammation
How Does Autologous Coronary Artery Atherosclerosis Develop?
Autologous coronary artery atherosclerosis develops through a series of stages. While the exact mechanisms are complex, the process generally follows these key steps:
SEE ALSO: How Long Can You Live with Cardiac Cachexia?
1. Endothelial Dysfunction
The endothelium is the inner lining of blood vessels that helps regulate blood flow and keeps the arteries smooth and flexible. In the early stages of atherosclerosis, the endothelium becomes damaged or dysfunctional due to factors like:
- High blood pressure (hypertension)
- High cholesterol levels
- Smoking
- Diabetes
When the endothelium is damaged, it becomes permeable, allowing lipids like low-density lipoprotein (LDL) cholesterol to penetrate the arterial wall.
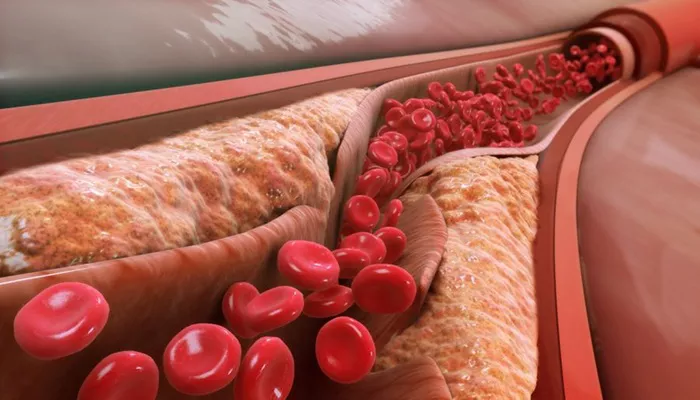
2. Lipid Accumulation and Oxidation
Once LDL cholesterol enters the arterial wall, it undergoes a process called oxidation. Oxidized LDL is highly inflammatory and triggers the immune system to respond. This begins the buildup of fatty streaks, which are the earliest form of plaque in the arteries.
Over time, these fatty streaks grow into larger plaques, consisting not only of lipids but also of dead cells, calcium, and scar tissue.
3. Inflammatory Response
The body’s immune system reacts to oxidized LDL by sending macrophages—a type of white blood cell—to the site of lipid accumulation. These macrophages try to clear away the cholesterol but often become overwhelmed, transforming into foam cells. Foam cells are lipid-laden macrophages that become a major component of the developing plaque.
The continuous presence of these immune cells and inflammatory mediators worsens the damage to the artery, contributing to the growth and instability of the plaque.
4. Plaque Growth and Complications
As plaque builds up, it narrows the artery, restricting blood flow to the heart muscle. At this stage, the individual may begin to experience symptoms like angina (chest pain) during physical exertion.
The plaque can also become unstable, meaning it is prone to rupture. If a plaque ruptures, it can form a blood clot that blocks the coronary artery entirely, leading to a myocardial infarction (heart attack). This is one of the most severe complications of coronary artery atherosclerosis.
Risk Factors for Autologous Coronary Artery Atherosclerosis
Several risk factors contribute to the development of autologous coronary artery atherosclerosis, many of which are related to lifestyle and genetic predisposition. These risk factors include:
1. High Cholesterol
Elevated levels of LDL cholesterol are one of the primary drivers of plaque formation. LDL is often referred to as “bad cholesterol” because it contributes to plaque buildup in the arteries. On the other hand, high-density lipoprotein (HDL) cholesterol is considered “good cholesterol” because it helps remove LDL from the bloodstream.
2. Hypertension
High blood pressure puts extra strain on the arterial walls, making them more susceptible to damage and plaque formation.
Over time, this added pressure accelerates the progression of atherosclerosis.
3. Smoking
Cigarette smoking is a major risk factor for atherosclerosis. The toxins in tobacco smoke damage the endothelium, increase cholesterol levels, and promote inflammation within the arteries.
4. Diabetes
People with diabetes have an increased risk of atherosclerosis due to elevated blood sugar levels, which can damage the blood vessels and lead to the accumulation of plaque.
5. Obesity and Sedentary Lifestyle
Being overweight or obese, particularly with excess fat around the abdomen, increases the risk of developing coronary artery atherosclerosis. A sedentary lifestyle further exacerbates this risk, as physical inactivity contributes to high blood pressure, diabetes, and unhealthy cholesterol levels.
6. Family History
Genetics play a significant role in the development of atherosclerosis.
A family history of coronary artery disease or heart attacks increases the likelihood that an individual will develop atherosclerosis, especially at an earlier age.
Symptoms of Autologous Coronary Artery Atherosclerosis
Many people with autologous coronary artery atherosclerosis may not experience symptoms until the condition has advanced. The most common symptoms include:
Angina: A pressing or squeezing pain in the chest that often occurs with physical activity or emotional stress.
Shortness of Breath: Reduced blood flow to the heart can cause the heart to work harder, leading to difficulty breathing.
Fatigue: Decreased oxygen delivery to the heart and body can lead to feelings of weakness and fatigue, especially during physical exertion.
Heart Attack Symptoms: In the case of plaque rupture and complete blockage of a coronary artery, symptoms may include severe chest pain, shortness of breath, sweating, and nausea.
Diagnosis of Coronary Artery Atherosclerosis
The diagnosis of autologous coronary artery atherosclerosis is based on a combination of clinical symptoms, risk factors, and diagnostic tests. Common tests used to diagnose this condition include:
Electrocardiogram (ECG): Measures the electrical activity of the heart and can detect areas of reduced blood flow.
Stress Testing: Evaluates the heart’s function during physical stress or with the use of medication to simulate stress.
Echocardiogram: Uses ultrasound to visualize the heart’s structure and function.
Coronary Angiography: A more invasive procedure that involves injecting a dye into the coronary arteries to visualize blockages on X-ray.
Blood Tests: Check for markers of heart damage, such as troponin, and assess cholesterol levels.
Treatment Options for Autologous Coronary Artery Atherosclerosis
Treatment for autologous coronary artery atherosclerosis focuses on managing symptoms, reducing risk factors, and preventing complications like heart attacks. Treatment options include:
1. Lifestyle Modifications
Diet: A heart-healthy diet low in saturated fats, cholesterol, and sodium can help reduce plaque buildup.
Exercise: Regular physical activity improves cardiovascular health and reduces many risk factors for atherosclerosis.
Smoking Cessation: Quitting smoking is one of the most important steps in reducing the risk of coronary artery disease.
2. Medications
Several medications are used to manage atherosclerosis, including:
Statins: Lower LDL cholesterol levels and stabilize plaques.
Antiplatelet Drugs: Reduce the risk of blood clots forming on existing plaques.
Beta-blockers and ACE inhibitors: Lower blood pressure and reduce strain on the heart.
3. Surgical Interventions
In advanced cases, surgical procedures may be necessary to restore blood flow to the heart, such as:
Angioplasty and Stenting: A balloon is used to open up the blocked artery, and a stent is placed to keep it open.
Coronary Artery Bypass Grafting (CABG): A surgical procedure that creates a bypass around the blocked section of the artery using a blood vessel from another part of the body.
Conclusion
Autologous coronary artery atherosclerosis is a complex, progressive condition driven by the body’s own metabolic processes. It results in plaque buildup within the coronary arteries, leading to restricted blood flow to the heart and potentially life-threatening complications. Understanding the risk factors and taking steps to manage them through lifestyle changes, medications, and, in some cases, surgery is critical for preventing heart attacks and improving overall heart health.
Related topics:
- How Long Can You Live with Chronic Atrial Fibrillation
- How Do Carotid Arteries Get Blocked?
- How Much Carotid Artery Blockage Is Normal?