Heart failure is a condition where the heart becomes weakened and cannot pump blood effectively throughout the body.
This can lead to fluid buildup, shortness of breath, fatigue, and other complications. One class of medications that has proven to be very effective in treating heart failure is angiotensin II receptor blockers (ARBs). In this article, we will explore what ARBs are, how they work, and how they benefit patients with heart failure.
What Are ARBs?
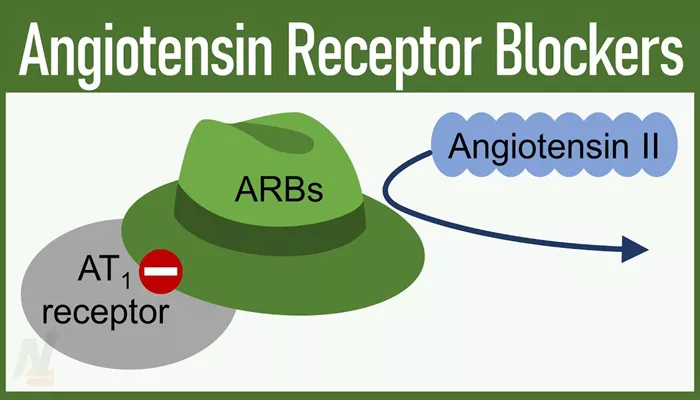
Angiotensin II receptor blockers, or ARBs, are a group of medications that help to relax blood vessels. They do this by blocking the effects of a hormone called angiotensin II. Angiotensin II narrows blood vessels, which increases blood pressure and forces the heart to work harder. ARBs prevent this hormone from binding to its receptors, allowing blood vessels to remain relaxed and open.
Some common ARBs include:
- Losartan
- Valsartan
- Irbesartan
- Candesartan
- Telmisartan
ARBs are primarily used to treat high blood pressure, but they are also prescribed for heart failure. By reducing the stress on the heart, they help improve the heart’s ability to pump blood and can reduce symptoms in heart failure patients.
The Role of the Renin-Angiotensin System (RAS) in Heart Failure
To understand how ARBs help heart failure, it is important to understand the role of the renin-angiotensin system (RAS) in regulating blood pressure and fluid balance. The RAS is a hormone system that regulates blood pressure and fluid levels in the body. When blood volume is low, the kidneys release an enzyme called renin. Renin converts angiotensinogen, a protein produced by the liver, into angiotensin I. Angiotensin I is then converted to angiotensin II by an enzyme called angiotensin-converting enzyme (ACE).
SEE ALSO: What Does Carpal Tunnel Syndrome Have to Do with Heart Failure
Angiotensin II is a powerful vasoconstrictor, meaning it causes blood vessels to narrow, which raises blood pressure. It also stimulates the release of aldosterone, a hormone that causes the kidneys to retain sodium and water. This increases blood volume, leading to higher blood pressure. While this system is helpful when the body needs to increase blood pressure, it can be problematic in heart failure because it adds more strain to an already weakened heart.
How Do ARBs Work in Heart Failure?
In heart failure, the body often activates the RAS to compensate for the heart’s reduced ability to pump blood. While this is initially helpful, prolonged activation of the RAS can lead to further damage to the heart and blood vessels. This is where ARBs come into play.
1. Blocking Harmful
Effects of Angiotensin II ARBs block the receptors that angiotensin II binds to. By doing so, they prevent the hormone from constricting blood vessels. This leads to vasodilation, or widening of the blood vessels, which helps to reduce blood pressure. With lower blood pressure, the heart does not have to work as hard to pump blood, which can reduce symptoms of heart failure and improve the quality of life for patients.
2. Reducing Fluid Retention
By blocking the effects of angiotensin II, ARBs also reduce the release of aldosterone. This helps to prevent sodium and water retention, which can lead to fluid buildup in the lungs, abdomen, and other parts of the body in heart failure patients.
By reducing fluid retention, ARBs help to relieve symptoms such as swelling (edema) and shortness of breath.
3. Protecting the Heart Muscle
Prolonged activation of the RAS can lead to structural changes in the heart, such as thickening of the heart muscle and scarring. These changes can further weaken the heart’s ability to pump blood. ARBs help to prevent these harmful changes by blocking the effects of angiotensin II, which can protect the heart muscle and improve long-term outcomes for heart failure patients.
Benefits of ARBs in Heart Failure
1. Improved Symptoms
One of the primary benefits of ARBs in heart failure is the improvement of symptoms. Patients with heart failure often experience shortness of breath, fatigue, and swelling due to the reduced ability of the heart to pump blood. By relaxing blood vessels and reducing fluid retention, ARBs can help to relieve these symptoms, making it easier for patients to perform daily activities.
2. Reduced Hospitalizations
Heart failure is a chronic condition that often requires frequent hospitalizations due to exacerbations of symptoms. Studies have shown that ARBs can reduce the risk of hospitalization in heart failure patients by helping to stabilize the condition and prevent acute episodes. This not only improves the quality of life for patients but also reduces the burden on healthcare systems.
3. Improved Survival Rates
Long-term studies have shown that ARBs can improve survival rates in patients with heart failure. By reducing the strain on the heart and preventing structural damage, these medications can help to prolong life and reduce the risk of complications such as heart attacks and strokes.
How Are ARBs Different From ACE Inhibitors?
ACE inhibitors are another class of medications that target the RAS, and they work by preventing the conversion of angiotensin I to angiotensin II. While both ARBs and ACE inhibitors are effective in treating heart failure, there are some differences between the two.
1. Cough Side Effect
One of the common side effects of ACE inhibitors is a persistent dry cough, which occurs in some patients. This is due to the accumulation of a substance called bradykinin, which is broken down by the same enzyme that converts angiotensin I to angiotensin II. ARBs do not affect bradykinin levels, so they are less likely to cause this side effect. For patients who cannot tolerate ACE inhibitors due to a cough, ARBs are often a suitable alternative.
2. Angioedema Risk
Angioedema, or swelling of the deeper layers of the skin, is a rare but serious side effect of ACE inhibitors. ARBs have a lower risk of causing angioedema, making them a safer option for some patients. However, patients who have experienced angioedema with ACE inhibitors should still be monitored closely if switched to an ARB.
When Are ARBs Prescribed for Heart Failure?
ARBs are typically prescribed for heart failure patients who cannot tolerate ACE inhibitors due to side effects such as a persistent cough or angioedema. They may also be used in combination with other heart failure medications, such as beta-blockers and diuretics, to provide comprehensive management of the condition.
The choice of ARB and the dosage will depend on the individual patient’s condition, overall health, and response to treatment. It is important for patients to take the medication exactly as prescribed and to report any side effects to their healthcare provider.
Conclusion
Angiotensin II receptor blockers (ARBs) are an effective treatment option for patients with heart failure. By blocking the effects of angiotensin II, these medications help to relax blood vessels, reduce fluid retention, and protect the heart muscle.
This leads to improved symptoms, fewer hospitalizations, and better long-term outcomes for patients. While ACE inhibitors are often the first choice for treating heart failure, ARBs are a valuable alternative for those who cannot tolerate ACE inhibitors or require additional treatment.
Related topics:
- Why Are Beta-Blockers Contraindicated in Heart Failure?
- How Does Kidney Failure Affect The Heart?
- Why Does Meth Cause Heart Failure?