Thrombolytic therapy plays a crucial role in the management of acute coronary syndromes (ACS), particularly during myocardial infarctions (heart attacks). The primary goal of thrombolytic therapy is to dissolve blood clots that obstruct blood flow to the heart muscle. By restoring blood flow, this therapy aims to minimize damage to the heart tissue and improve patient outcomes. However, while thrombolytic therapy can be life-saving, it is not without risks. One significant complication associated with thrombolytic therapy is the development of arrhythmias.
Arrhythmias are irregular heartbeats that can lead to serious complications, including cardiac arrest. Understanding how thrombolytic therapy contributes to the onset of arrhythmias is essential for healthcare providers to manage risks effectively. This article explores the mechanisms by which thrombolytic therapy can lead to arrhythmias, the types of arrhythmias that may occur, risk factors, and strategies for monitoring and managing these complications.
Mechanisms of Arrhythmia Induction
Thrombolytic therapy can induce arrhythmias through various mechanisms. Here are the primary pathways involved:
1. Restoration of Blood Flow
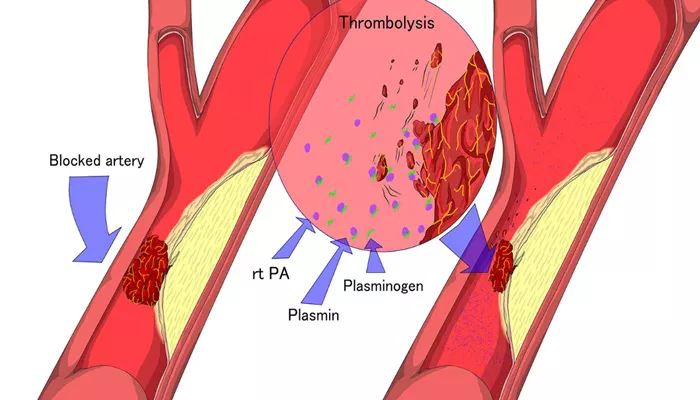
Thrombolytic agents work by breaking down fibrin, the protein that forms the backbone of blood clots. When a clot is dissolved, blood flow is restored to previously ischemic heart tissue. However, the sudden influx of blood can lead to a rapid change in the myocardial environment, which can trigger electrical disturbances.
The restoration of blood flow may result in:
Reperfusion Injury: This phenomenon occurs when blood supply returns to tissue after a period of ischemia. The sudden reintroduction of oxygen can cause oxidative stress, leading to cell damage. This damage can disrupt the normal electrical conduction pathways of the heart, leading to arrhythmias.
Changes in Ion Concentrations: Restoration of blood flow can alter the concentrations of key ions (such as potassium, calcium, and magnesium) within the heart muscle. These changes can disrupt the delicate balance required for normal electrical activity and result in arrhythmias.
2. Electrical Instability
Ischemic heart tissue is often electrically unstable. Thrombolytic therapy can exacerbate this instability by causing:
Early Afterdepolarizations (EADs): These are abnormal depolarizations that occur during the repolarization phase of the cardiac action potential. EADs can be triggered by changes in ion concentrations and lead to arrhythmias, particularly in the context of restored blood flow.
Delayed Afterdepolarizations (DADs): DADs occur when there is an influx of calcium ions into the cardiac cells, usually due to sarcoplasmic reticulum overload. Thrombolytic therapy can increase calcium availability in the ischemic myocardium, leading to DADs and subsequent arrhythmias.
3. Ventricular Wall Stress
After thrombolysis, the heart must pump against a higher workload as blood flow resumes. This can lead to mechanical stress on the ventricular walls. Increased wall stress can trigger electrical disturbances through mechanisms such as:
Stretch-induced Arrhythmias: The rapid expansion of heart muscle fibers can create mechanical tension, leading to alterations in electrical conduction. Stretching the myocardial fibers can enhance automaticity and disrupt the normal conduction pathways, increasing the risk of arrhythmias.
4. Inflammatory Response
Thrombolytic therapy can trigger an inflammatory response within the heart and surrounding tissues. This inflammation can contribute to arrhythmias through several mechanisms:
Cytokine Release: Thrombolytic therapy can lead to the release of inflammatory cytokines, which may affect myocardial excitability and conduction properties.
Fibrosis: Inflammatory processes can contribute to structural changes within the heart, such as fibrosis. Fibrosis disrupts the normal conduction pathways and can serve as a substrate for arrhythmias.
Types of Arrhythmias Associated with Thrombolytic Therapy
Arrhythmias can be classified based on their origin and characteristics. The following are common types of arrhythmias associated with thrombolytic therapy:
SEE ALSO: What Are Heart Flutters Caused by?
1. Atrial Fibrillation
Atrial fibrillation (AF) is a common arrhythmia characterized by rapid and irregular electrical activity in the atria. AF can be triggered by the changes in hemodynamics and electrolyte imbalances that occur during and after thrombolytic therapy.
The presence of AF can lead to increased heart rates and may result in further complications, including stroke.
2. Ventricular Tachycardia (VT)
Ventricular tachycardia is a potentially life-threatening arrhythmia that arises from abnormal electrical activity in the ventricles. VT can occur due to:
Reperfusion Injury: As previously mentioned, reperfusion injury can lead to electrical instability in the heart, predisposing patients to VT.
Structural Changes: Patients may already have structural heart disease, and thrombolytic therapy can exacerbate pre-existing conditions that promote VT.
3. Ventricular Fibrillation (VF)
Ventricular fibrillation is a critical condition in which the ventricles quiver ineffectively instead of pumping blood. This arrhythmia is a medical emergency and can lead to cardiac arrest. The risk of VF increases with:
Severe Ischemia: If thrombolytic therapy is delayed or if there is extensive myocardial damage, the risk of VF increases.
Electrolyte Imbalances: Imbalances caused by thrombolytic therapy may also predispose patients to VF.
4. Premature Ventricular Contractions (PVCs)
PVCs are early heartbeats originating from the ventricles. They can be benign but may also indicate underlying heart disease. Thrombolytic therapy can increase the frequency of PVCs due to the aforementioned mechanisms of reperfusion and electrical instability.
Risk Factors for Arrhythmias in Thrombolytic Therapy
Several factors can increase the likelihood of developing arrhythmias during thrombolytic therapy:
Patient History: A history of prior arrhythmias, coronary artery disease, or heart failure can increase risk.
Age: Older patients are at higher risk for arrhythmias due to age-related changes in the cardiovascular system.
Electrolyte Imbalances: Pre-existing imbalances in potassium, magnesium, or calcium can predispose patients to arrhythmias.
Heart Rate Variability: Increased heart rate variability after thrombolytic therapy can be a risk factor for developing arrhythmias.
Monitoring And Management
Effective monitoring and management strategies are essential to minimize the risk of arrhythmias during thrombolytic therapy. These include:
1. Continuous Cardiac Monitoring
Patients receiving thrombolytic therapy should be closely monitored using continuous electrocardiography (ECG). This allows for the early detection of arrhythmias, enabling prompt intervention.
2. Electrolyte Management
Regular monitoring of serum electrolytes, particularly potassium and magnesium, is crucial. Correcting any imbalances can help mitigate the risk of arrhythmias.
3. Use of Antiarrhythmic Medications
In patients with a history of arrhythmias or those who develop arrhythmias during thrombolytic therapy, the use of antiarrhythmic medications may be necessary. Commonly used agents include:
Beta-Blockers: These can help stabilize heart rhythm and reduce heart rate.
Calcium Channel Blockers: These can help manage atrial fibrillation and control ventricular rate.
4. Defibrillator Preparedness
For patients at high risk for life-threatening arrhythmias, access to defibrillation equipment should be readily available.
This may involve using an automated external defibrillator (AED) in emergency situations.
Conclusion
Thrombolytic therapy is a vital treatment for patients experiencing myocardial infarctions. While it is effective in restoring blood flow and reducing heart muscle damage, it can also lead to significant complications, including arrhythmias.
Understanding the mechanisms by which thrombolytic therapy induces arrhythmias is critical for healthcare providers.
By monitoring patients closely and implementing appropriate management strategies, the risks associated with arrhythmias can be minimized. Further research is necessary to enhance our understanding of thrombolytic therapy’s effects and improve patient safety in clinical practice.
Related topics:
- What Makes Arrhythmia Worse?
- How Long Does It Take for Arrhythmia to Go Away?
- What Type of Arrhythmia Causes Cardiac Arrest?