Ischemia and arrhythmia are two terms that frequently come up in discussions about heart health, but many people are unaware of how closely they are related. Ischemia occurs when there is a reduction in blood flow to the heart muscle, often due to a partial or complete blockage of the coronary arteries. This reduced blood flow means that the heart muscle does not get enough oxygen and nutrients to function properly. On the other hand, arrhythmia refers to irregularities in the heart’s rhythm. While there are many causes of arrhythmia, ischemia is one of the most significant factors. Understanding how ischemia can lead to arrhythmia is essential for managing heart health, particularly in individuals at risk of heart disease.
What Is Ischemia?
Ischemia occurs when the blood flow to a part of the body is reduced, preventing the tissues from getting the oxygen and nutrients they need to function correctly. In the context of the heart, ischemia happens when the coronary arteries—responsible for supplying blood to the heart muscle—become narrowed or blocked. This blockage can be caused by atherosclerosis, where fatty deposits build up on the walls of the arteries, leading to reduced blood flow. Ischemia can be temporary, such as during physical exertion or stress, or it can be more persistent and severe, increasing the risk of a heart attack.
When the heart muscle experiences ischemia, it struggles to pump efficiently because it is deprived of oxygen. Without enough oxygen, the cells in the heart muscle cannot produce the energy they need to contract and relax normally. This can lead to a variety of complications, including angina (chest pain), heart attack, and arrhythmia.
What Is Arrhythmia?
Arrhythmia is a condition where the heart beats too fast, too slow, or irregularly. The heart’s normal rhythm is controlled by electrical signals that coordinate the contraction and relaxation of the heart muscle.
When these signals are disrupted, the heart may not beat in a regular, coordinated manner. Arrhythmias can range from mild and harmless to severe and life-threatening. Common types of arrhythmias include:
Tachycardia: A fast heart rate, usually over 100 beats per minute.
Bradycardia: A slow heart rate, usually below 60 beats per minute.
Atrial fibrillation: An irregular and often rapid heart rate that can lead to blood clots, stroke, and other complications.
Ventricular fibrillation: A rapid, chaotic heart rhythm that can be fatal if not treated immediately.
The Link Between Ischemia And Arrhythmia
Ischemia and arrhythmia are closely linked because reduced blood flow to the heart muscle can affect the electrical signals that regulate the heart’s rhythm. When the heart does not receive enough oxygen due to ischemia, several changes occur within the heart muscle cells that can lead to arrhythmia. These changes include:
Altered Ion Channels:
The heart’s electrical activity is controlled by the movement of ions (such as sodium, potassium, and calcium) across the cell membranes of heart muscle cells. These ions create electrical impulses that trigger the heart to contract and relax in a coordinated manner.
Ischemia affects the function of ion channels, which are proteins that regulate the flow of ions into and out of the cells.
When blood flow is reduced, the balance of ions is disrupted, leading to abnormal electrical activity. This can cause the heart to beat irregularly.
Acidosis and Changes in pH:
During ischemia, the lack of oxygen causes the heart muscle cells to switch from aerobic (oxygen-dependent) metabolism to anaerobic (without oxygen) metabolism. This process produces lactic acid, leading to a condition known as acidosis.
Acidosis alters the electrical properties of the heart muscle cells, making them more prone to abnormal electrical impulses.
This can contribute to the development of arrhythmias, especially during periods of severe ischemia.
SEE ALSO: What Type of Arrhythmia Causes Cardiac Arrest?
Reduced Cellular Energy:
Heart muscle cells rely on a steady supply of oxygen to produce energy in the form of adenosine triphosphate (ATP). ATP is necessary for the proper functioning of ion channels and for maintaining the normal electrical activity of the heart.
When ischemia occurs, the production of ATP decreases, leading to energy depletion in the heart muscle cells. This energy deficit can cause the cells to become electrically unstable, increasing the likelihood of arrhythmias.
Structural Damage to the Heart Muscle:
If ischemia is prolonged, it can lead to damage or death of heart muscle cells (myocardial infarction or heart attack). This damage creates areas of scar tissue that do not conduct electrical signals properly, disrupting the normal flow of electrical impulses across the heart.
Scar tissue can create a phenomenon known as re-entry, where electrical impulses loop around the damaged area, causing the heart to beat abnormally fast or irregularly. Re-entry is a common mechanism underlying many types of arrhythmias, including ventricular tachycardia and atrial fibrillation.
Mechanisms by Which Ischemia Triggers Arrhythmia
1. Direct Effects on Electrical Conduction
The heart’s electrical conduction system consists of specialized cells that transmit electrical impulses throughout the heart.
These impulses ensure that the heart contracts and relaxes in a coordinated manner.
During ischemia, the reduced oxygen supply affects the ability of these cells to transmit electrical signals effectively. This disruption can lead to slowed conduction, re-entry circuits, and abnormal heartbeats. In some cases, ischemia can cause the heart to develop a rhythm known as ventricular tachycardia, which is characterized by a rapid heartbeat originating from the ventricles.
2. Changes in Autonomic Nervous System Activity
The autonomic nervous system, which controls involuntary bodily functions, plays a critical role in regulating heart rate and rhythm.
Ischemia can cause an imbalance in the activity of the sympathetic and parasympathetic branches of the autonomic nervous system. The sympathetic nervous system, responsible for the “fight or flight” response, can become overactive during ischemic episodes, leading to increased heart rate and excitability of the heart muscle. This heightened excitability can make the heart more susceptible to arrhythmias.
3. Development of Ischemic Preconditioning
Interestingly, repeated episodes of brief ischemia can lead to a phenomenon known as ischemic preconditioning. In this process, the heart becomes more resistant to the effects of future ischemic events.
While ischemic preconditioning may offer some protective effects against heart attacks, it does not completely eliminate the risk of arrhythmia. In fact, during the early stages of ischemic preconditioning, the heart may be more prone to developing arrhythmias due to the temporary imbalance in electrical activity.
Clinical Implications
Understanding how ischemia causes arrhythmia has important implications for the diagnosis, treatment, and prevention of heart rhythm disorders. For individuals with coronary artery disease, managing risk factors such as high blood pressure, high cholesterol, and diabetes is crucial for reducing the likelihood of ischemic episodes. Treatments aimed at improving blood flow to the heart, such as medications, angioplasty, and coronary artery bypass surgery, can help reduce the risk of both ischemia and arrhythmia.
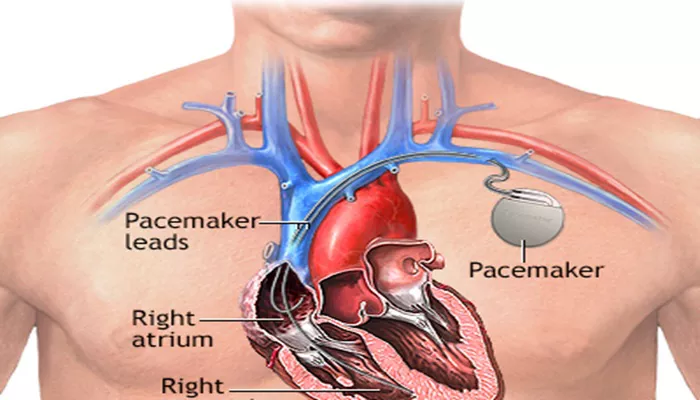
In cases where arrhythmias do occur, treatment options may include medications (such as beta-blockers and antiarrhythmics), implantable devices (such as pacemakers and defibrillators), and catheter ablation procedures that target abnormal electrical pathways in the heart. For patients with recurrent or severe arrhythmias, comprehensive cardiac care that addresses both ischemic heart disease and arrhythmia is essential.
Conclusion
Ischemia and arrhythmia are closely intertwined, with reduced blood flow to the heart muscle leading to a range of changes that can disrupt the heart’s normal electrical activity. By understanding the mechanisms through which ischemia triggers arrhythmias, healthcare providers can better manage and treat these conditions, ultimately improving outcomes for patients with heart disease.
Related topics:
- How Does Thrombolysis Treatment Cause Arrhythmias?
- What Makes Arrhythmia Worse?
- How Long Does It Take for Arrhythmia to Go Away?