Myocarditis is an inflammatory condition affecting the heart muscle, known as the myocardium. This inflammation can interfere with the heart’s ability to pump blood effectively and may lead to various cardiac symptoms, including an abnormal heart rate. Understanding how myocarditis affects your heart rate is essential for recognizing the condition and seeking timely treatment. This article provides a detailed overview of what happens to your heart rate when you have myocarditis, its underlying causes, symptoms, and treatment options.
What Is Myocarditis?
Myocarditis refers to inflammation of the myocardium, which is the thick muscular layer of the heart wall responsible for contracting and propelling blood throughout the body. The condition can be caused by various factors, including viral infections, bacterial infections, autoimmune diseases, toxins, and other inflammatory conditions. Viruses like Coxsackievirus B, adenovirus, and parvovirus B19 are some of the most common culprits.
The severity of myocarditis can range from mild to life-threatening. In mild cases, people might not even realize they have myocarditis because symptoms can be subtle or absent. However, severe cases may lead to serious complications, including heart failure, arrhythmias, and even sudden cardiac arrest.
What Happens to Your Heart Rate When You Have Myocarditis?
Myocarditis can cause changes in your heart rate, ranging from increased to irregular heartbeats. Let’s look at how the condition can affect your heart rate:
Tachycardia (Increased Heart Rate)
One of the most common effects of myocarditis is tachycardia, a condition characterized by a faster-than-normal heart rate.
For adults, a resting heart rate above 100 beats per minute (bpm) is generally considered tachycardia. In individuals with myocarditis, tachycardia often occurs because the inflamed heart muscle is less efficient at pumping blood. To compensate, the heart speeds up its rhythm to meet the body’s demand for oxygen and nutrients.
The increased heart rate can make individuals feel palpitations, or the sensation of a racing heart. It is a response to the stress and inflammation within the heart muscle, but this increased workload can further damage the heart, especially if the myocarditis is not treated promptly.
Bradycardia (Decreased Heart Rate)
While less common, some individuals with myocarditis may experience bradycardia, which is a slower-than-normal heart rate. For adults, a resting heart rate below 60 bpm is typically considered bradycardia. This condition might occur if the inflammation affects the electrical pathways that control the heart’s rhythm, leading to a slower and more irregular heartbeat. Bradycardia can result in dizziness, fatigue, or even fainting if the heart cannot pump enough blood to meet the body’s needs.
Arrhythmias (Irregular Heartbeats)
Myocarditis can also cause arrhythmias, or irregular heartbeats. These may include premature beats, atrial fibrillation (rapid and irregular beating of the upper chambers of the heart), or ventricular arrhythmias (rapid beating of the lower chambers).
Arrhythmias can be serious and sometimes life-threatening, depending on their type and severity.
In myocarditis, arrhythmias may arise due to the inflammation disrupting the heart’s electrical system. This disruption can cause the heart to beat irregularly, skip beats, or beat erratically, leading to symptoms such as palpitations, chest discomfort, shortness of breath, and lightheadedness.
Why Does Myocarditis Affect Heart Rate?
To understand why myocarditis affects heart rate, it’s important to understand how the heart functions. The myocardium plays a vital role in contracting and relaxing, enabling the heart to pump blood. In myocarditis, the inflammation causes the muscle cells to swell and weaken, leading to a decrease in the heart’s ability to contract efficiently.
Inflammation And Heart Function
The inflammation associated with myocarditis can have several effects on the heart muscle:
Damage to Muscle Cells: Inflammation can damage the myocardial cells, reducing their ability to contract properly. When the heart struggles to pump blood, it compensates by increasing its rate of contraction, leading to tachycardia.
Swelling and Stiffness: The swelling of the heart muscle makes it stiffer and less flexible, impeding its ability to fill with and eject blood efficiently. This increased workload can cause the heart to beat faster.
Disruption of Electrical Pathways: The inflammation may interfere with the heart’s electrical system, which coordinates the heartbeat. Disruptions in these pathways can cause irregular heart rhythms, contributing to arrhythmias or even bradycardia if the electrical signals are blocked or delayed.
Symptoms Associated with Heart Rate Changes in Myocarditis
The changes in heart rate caused by myocarditis can lead to various symptoms, including:
Palpitations: The sensation of a racing, pounding, or fluttering heartbeat.
Fatigue: A feeling of extreme tiredness, often due to the heart’s inability to pump blood efficiently.
Shortness of Breath: Difficulty breathing, especially during physical activity or when lying down.
Dizziness or Lightheadedness: Feeling faint or unsteady, which can occur if the heart does not pump enough blood to the brain.
Chest Pain: A sharp or dull pain in the chest, which may worsen with physical activity.
If you experience any of these symptoms, especially if they occur suddenly or worsen, it is crucial to seek medical attention immediately.
Diagnosing Myocarditis And Its Effect on Heart Rate
Diagnosis of myocarditis typically involves a combination of medical history, physical examination, and diagnostic tests. If myocarditis is suspected, a healthcare provider may use the following tests to assess heart function and determine the impact on heart rate:
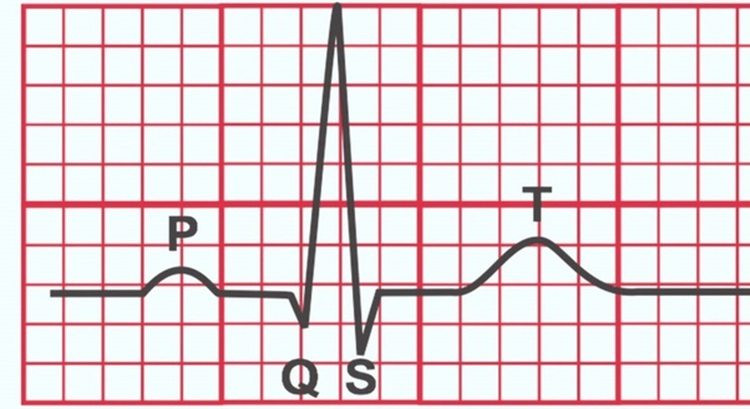
Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart and can detect abnormal heart rhythms, which may suggest myocarditis.
Echocardiogram: An ultrasound of the heart that helps visualize the heart’s structure and function. It can reveal changes in heart size, wall motion, and pumping ability.
Cardiac MRI: This imaging test provides a detailed view of the heart’s tissues, which can show signs of inflammation and swelling, helping to confirm the diagnosis of myocarditis.
Blood Tests: Blood tests can identify markers of inflammation and infection, such as elevated levels of C-reactive protein (CRP) or troponin, a protein released when the heart muscle is damaged.
Holter Monitor: A portable device worn for 24-48 hours to record heart rhythms continuously, helping detect intermittent arrhythmias.
Conclusion
Myocarditis can significantly impact your heart rate, leading to tachycardia, bradycardia, or arrhythmias. These changes occur because inflammation damages the heart muscle, affects its pumping efficiency, and disrupts the heart’s electrical pathways. Understanding the effects of myocarditis on heart rate can help in recognizing the condition early and seeking appropriate treatment. If you experience symptoms such as palpitations, shortness of breath, or dizziness, consult a healthcare professional promptly.
Related topics: