Junctional arrhythmia is a type of heart rhythm disorder that originates in the junctional tissue of the heart, specifically the area between the atria (the upper chambers) and the ventricles (the lower chambers). This condition can disrupt the normal electrical conduction of the heart, leading to various symptoms and potential complications. Understanding junctional arrhythmia is essential for both patients and healthcare providers, as it can have implications for heart health and overall well-being.
In this article, we will explore the causes, types, symptoms, diagnosis, and treatment options for junctional arrhythmia. We will break down complex concepts into simpler terms to ensure a comprehensive understanding of this condition.
What Causes Junctional Arrhythmia?
Junctional arrhythmia can arise from several factors that affect the heart’s electrical system. These causes can be broadly categorized into structural and functional issues.
Structural Causes
Heart Disease: Conditions such as coronary artery disease or cardiomyopathy can lead to changes in the heart’s structure, impacting electrical conduction.
Congenital Defects: Some individuals may be born with heart defects that affect the junctional area.
Myocarditis: Inflammation of the heart muscle can disrupt normal electrical activity.
Heart Surgery: Surgical procedures on the heart may inadvertently damage the electrical conduction pathways.
SEE ALSO: When Should I Go to The Hospital for Arrhythmia?
Functional Causes
Medications: Certain drugs, especially those affecting heart rate and rhythm, can induce junctional arrhythmias.
Electrolyte Imbalances: Abnormal levels of potassium, magnesium, or calcium can impact the heart’s electrical system.
Autonomic Nervous System Activity: Changes in nervous system activity, such as during stress or illness, can influence heart rhythms.
Hypoxia: Reduced oxygen levels in the blood can lead to arrhythmias.
Types of Junctional Arrhythmia
Junctional arrhythmias can be classified into several types, each characterized by its unique electrical patterns and clinical implications.
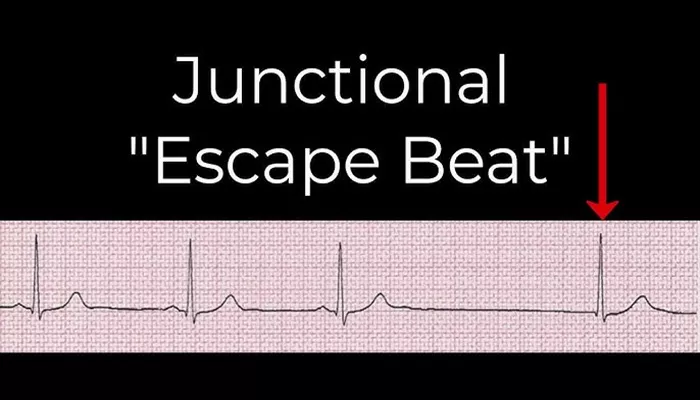
1. Junctional Escape Rhythm
A junctional escape rhythm occurs when the heart’s natural pacemaker (the sinoatrial node) fails to send signals. In this case, the junctional tissue takes over as the pacemaker. The heart rate is typically slower, ranging from 40 to 60 beats per minute.
2. Junctional Premature Beats (JPBs)
JPBs are early heartbeats that originate in the junctional area. They can occur in healthy individuals and are often benign.
However, frequent JPBs may signal underlying heart conditions.
3. Junctional Tachycardia
This type of arrhythmia occurs when the junctional tissue generates rapid impulses, leading to an increased heart rate. Junctional tachycardia can be symptomatic and may require intervention.
Symptoms of Junctional Arrhythmia
The symptoms of junctional arrhythmia can vary based on the type and severity of the condition. Some common symptoms include:
Palpitations: A feeling of skipped or rapid heartbeats.
Dizziness or Lightheadedness: Reduced blood flow can lead to feelings of faintness.
Fatigue: Decreased cardiac output can cause tiredness.
Shortness of Breath: Difficulty breathing, especially during exertion.
Chest Pain: In some cases, individuals may experience discomfort or pain in the chest.
Asymptomatic Cases
It is important to note that some individuals with junctional arrhythmia may be asymptomatic, meaning they do not experience any noticeable symptoms. Regular check-ups and monitoring can help identify these cases.
Diagnosis of Junctional Arrhythmia
Diagnosing junctional arrhythmia typically involves a combination of medical history, physical examination, and diagnostic tests.
1. Medical History
The healthcare provider will start by asking about symptoms, medical history, and any medications currently being taken.
This information is crucial for understanding the context of the arrhythmia.
2. Physical Examination
A physical exam will often include checking the pulse and listening to the heart. Irregularities in heart sounds or pulse can indicate an arrhythmia.
3. Electrocardiogram (ECG)
An ECG is the primary tool used to diagnose junctional arrhythmia. It records the electrical activity of the heart and can identify the type of arrhythmia present. The ECG will show specific patterns, such as the absence of P waves in the case of junctional escape rhythms.
4. Holter Monitor
If the arrhythmia is intermittent, a healthcare provider may recommend a Holter monitor. This portable device records the heart’s electrical activity over 24 to 48 hours, helping capture episodes of arrhythmia that may not occur during a standard ECG.
5. Other Tests
In some cases, additional tests such as echocardiograms, stress tests, or blood tests may be necessary to evaluate heart function and identify potential underlying causes.
Treatment Options for Junctional Arrhythmia
The treatment for junctional arrhythmia depends on the type, severity, and underlying causes. Options may include:
1. Observation
For asymptomatic cases or benign junctional premature beats, healthcare providers may recommend monitoring without immediate intervention. Regular follow-up visits can ensure that any changes in condition are promptly addressed.
2. Medications
In symptomatic cases, medications may be prescribed to help regulate heart rate and rhythm. Beta-blockers, calcium channel blockers, or antiarrhythmic drugs can be used depending on the specific situation.
3. Pacemaker Insertion
In cases of significant bradycardia (slow heart rate) or persistent junctional escape rhythms, a pacemaker may be necessary.
This device helps maintain a regular heart rate by providing electrical impulses to the heart.
4. Treating Underlying Conditions
If junctional arrhythmia is caused by an underlying condition, addressing that condition is crucial. For instance, correcting electrolyte imbalances or managing heart disease can improve arrhythmia symptoms.
5. Catheter Ablation
In cases of junctional tachycardia that are not responsive to medications, catheter ablation may be considered. This procedure involves using radiofrequency energy to destroy the small area of tissue responsible for the abnormal electrical impulses.
Living with Junctional Arrhythmia
For individuals diagnosed with junctional arrhythmia, lifestyle modifications may help manage symptoms and reduce the risk of complications. Recommendations may include:
Regular Monitoring: Keep track of heart rate and any symptoms to share with healthcare providers during visits.
Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains can promote heart health.
Regular Exercise: Engaging in regular physical activity, as advised by a healthcare provider, can help improve cardiovascular fitness.
Stress Management: Techniques such as meditation, yoga, or deep breathing can help manage stress levels, which may impact heart health.
Avoiding Stimulants: Reducing caffeine and other stimulants can minimize the risk of triggering arrhythmias.
Conclusion
Junctional arrhythmia is a condition that affects the heart’s electrical conduction system, potentially leading to various symptoms and complications. Understanding the causes, types, and treatment options available is vital for managing this condition effectively. If you or someone you know is experiencing symptoms of arrhythmia, seeking medical attention is essential for proper diagnosis and management.
Related topics: