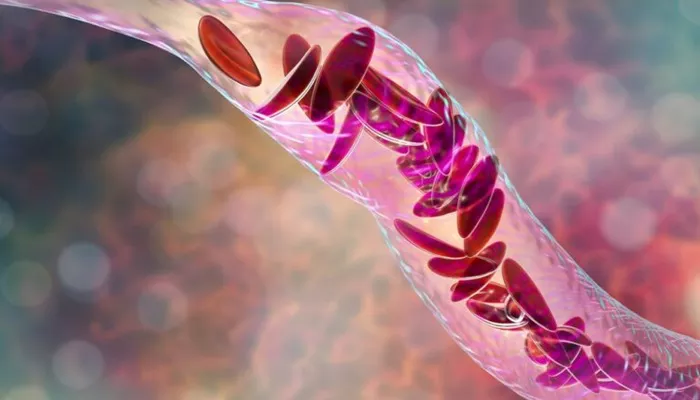
Sickle cell disease (SCD) is a genetic blood disorder characterized by the production of abnormal hemoglobin, known as hemoglobin S. This condition leads to the deformation of red blood cells into a crescent or “sickle” shape. Unlike normal red blood cells, which are flexible and disc-shaped, sickle cells are rigid and can become stuck in small blood vessels. This blockage can result in pain, organ damage, and a range of complications, including heart failure. Understanding the mechanisms by which sickle cells contribute to heart failure is crucial for improving treatment and patient outcomes.
Pathophysiology of Sickle Cell Disease
Abnormal Hemoglobin Production
In individuals with sickle cell disease, the mutation in the beta-globin gene leads to the production of hemoglobin S. When oxygen levels in the blood decrease, hemoglobin S polymerizes, causing red blood cells to distort into a sickle shape. This process not only reduces the cells’ ability to carry oxygen but also increases their tendency to clump together.
Microvascular Obstruction
Sickle-shaped cells can obstruct capillaries and small blood vessels, leading to a phenomenon known as vaso-occlusion.
This blockage causes ischemia (reduced blood flow) to various organs, including the heart. The heart requires a constant supply of oxygen-rich blood to function properly, and any interruption can lead to damage.
Hemolysis
Sickle cells have a shorter lifespan than normal red blood cells, typically lasting 10 to 20 days compared to 120 days for healthy cells. This increased destruction of red blood cells leads to hemolytic anemia, which can further exacerbate the heart’s workload. As the body tries to compensate for the lack of healthy red blood cells, the heart must pump harder, leading to increased strain.
The Link Between Sickle Cells And Heart Failure
Increased Cardiac Output
In response to anemia, the body often attempts to increase cardiac output to deliver more oxygen to tissues. This can lead to a condition known as high-output heart failure, where the heart is unable to sustain the increased demands placed upon it. The heart initially compensates by enlarging (dilated cardiomyopathy), but over time, this can lead to structural changes that impair function.
Right Heart Dysfunction
Sickle cell disease can lead to pulmonary hypertension, a condition where the blood pressure in the pulmonary arteries rises. The rigid sickle cells can cause damage to the small vessels in the lungs, leading to reduced oxygen exchange and increased pressure. The right side of the heart, which pumps blood to the lungs, must work harder to overcome this increased pressure, eventually leading to right heart failure.
Left Ventricular Hypertrophy
Chronic anemia and high-output demands can also result in left ventricular hypertrophy (LVH), where the muscle wall of the heart becomes thickened. This condition can lead to diastolic dysfunction, where the heart struggles to relax and fill with blood. Over time, this can progress to heart failure with preserved ejection fraction (HFpEF), where the heart maintains its pumping ability but fails to fill properly.
Arrhythmias
Sickle cell disease can also predispose patients to arrhythmias, or irregular heartbeats. The structural changes in the heart muscle, along with electrolyte imbalances caused by hemolysis, can disrupt the normal electrical conduction system of the heart. These arrhythmias can lead to palpitations, dizziness, and even sudden cardiac death.
Clinical Presentation of Heart Failure in Sickle Cell Disease
Symptoms
Patients with heart failure due to sickle cell disease may experience a variety of symptoms, including:
Shortness of breath, especially during physical activity
Fatigue and weakness
Swelling in the legs, ankles, or abdomen
Rapid or irregular heartbeat
Persistent cough or wheezing
SEE ALSO: How Does Losartan Help Heart Failure?
Diagnostic Tools
Early detection of heart failure in patients with sickle cell disease is vital for effective management. Several diagnostic tools can be employed, including:
Echocardiography: This imaging test uses sound waves to create images of the heart’s structure and function, allowing for assessment of chamber size, wall thickness, and ejection fraction.
Electrocardiogram (ECG): An ECG measures the heart’s electrical activity and can help identify arrhythmias or signs of hypertrophy.
B-type natriuretic peptide (BNP) testing: Elevated levels of BNP can indicate heart failure and are useful in monitoring the severity of the condition.
Management Strategies
Comprehensive Care Approach
Managing heart failure in patients with sickle cell disease requires a multidisciplinary approach. Key components of care include:
Hydration: Maintaining adequate hydration can help reduce sickling episodes and vaso-occlusion.
Pain management: Effective pain control is essential to improve quality of life and reduce stress on the heart.
Transfusion therapy: Regular blood transfusions can help alleviate anemia and reduce the proportion of sickle cells in circulation.
Pulmonary hypertension treatment: Medications such as endothelin receptor antagonists and phosphodiesterase-5 inhibitors can help manage pulmonary hypertension and improve right heart function.
Heart Failure Medications
Patients with heart failure may benefit from standard heart failure therapies, including:
Diuretics: These medications can help reduce fluid overload and swelling.
ACE inhibitors or ARBs: Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers can help lower blood pressure and reduce strain on the heart.
Beta-blockers: These medications can improve heart function and reduce the risk of arrhythmias.
Conclusion
Sickle cell disease is a complex condition that significantly impacts cardiovascular health. The abnormal shape of sickle cells leads to various complications, including heart failure. Understanding the mechanisms linking sickle cells to heart failure is essential for developing effective treatment strategies. Through comprehensive care, including hydration, pain management, and appropriate medications, healthcare providers can improve outcomes for patients with sickle cell disease and heart failure.
Related topics: