Heart failure is a complex clinical syndrome characterized by the heart’s inability to pump sufficient blood to meet the body’s needs. This condition can manifest in two primary forms: acute heart failure and chronic heart failure. Each type has distinct characteristics, causes, symptoms, and treatment strategies. Understanding these differences is crucial for effective diagnosis and management.
Introduction
Heart failure affects millions worldwide and is a leading cause of morbidity and mortality. The condition can arise from various underlying cardiovascular diseases, including coronary artery disease, hypertension, and valvular heart disease.
While both acute and chronic heart failure share some common symptoms, they differ significantly in their onset, progression, and clinical management. This article aims to elucidate the differences between acute and chronic heart failure, providing a detailed overview of their respective characteristics.
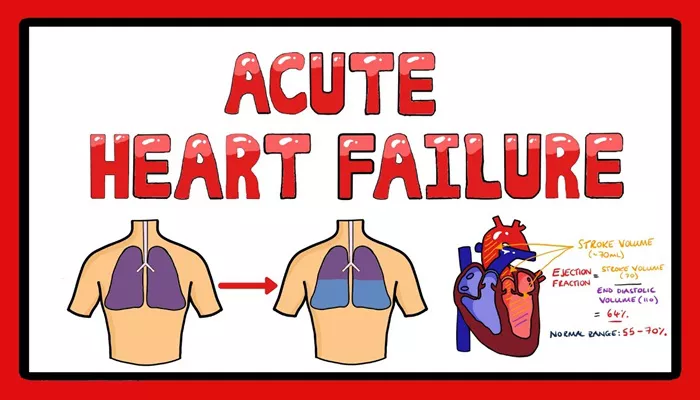
Definition of Acute Heart Failure
Acute heart failure (AHF) refers to the sudden onset or worsening of symptoms related to heart failure. It can occur in individuals with no prior history of heart problems (de novo heart failure) or in those with pre-existing chronic heart failure who experience an exacerbation (acute decompensated heart failure). AHF is often life-threatening and requires immediate medical intervention.
SEE ALSO: How Does Thiamine Deficiency Cause Heart Failure?
Symptoms of Acute Heart Failure
The symptoms of AHF typically develop rapidly and may include:
Severe shortness of breath (dyspnea), especially during physical activity or when lying flat.
Fluid retention, leading to swelling in the legs, ankles, or abdomen.
Rapid or irregular heartbeat (palpitations).
Coughing or wheezing, particularly when lying down.
Fatigue and weakness.
Confusion or altered mental state due to reduced blood flow to the brain.
Definition of Chronic Heart Failure
Chronic heart failure (CHF), often referred to as congestive heart failure, is a long-term condition that develops gradually over time. It results from the heart’s progressive inability to pump blood effectively, leading to inadequate oxygen delivery to tissues. CHF can be stable for extended periods but may also experience episodes of acute decompensation.
Symptoms of Chronic Heart Failure
Symptoms of CHF usually develop slowly and may include:
Persistent shortness of breath, especially during exertion or while lying flat.
Chronic fatigue and reduced exercise tolerance.
Swelling in the legs, ankles, or abdomen due to fluid buildup.
Coughing or wheezing, particularly at night.
Weight gain from fluid retention.
Key Differences Between Acute And Chronic Heart Failure
Understanding the distinctions between acute and chronic heart failure is essential for appropriate clinical management. Below are detailed comparisons based on various parameters:
| Feature | Acute Heart Failure | Chronic Heart Failure |
| Onset | Sudden onset; may occur within hours or days | Gradual onset; develops over months or years |
| Duration | Short-term; symptoms can improve rapidly with treatment | Long-term; symptoms persist and worsen over time |
| Severity of Symptoms | Severe symptoms requiring immediate intervention | Symptoms are often mild but can worsen episodically |
| Causes | Often precipitated by acute events (e.g., myocardial infarction) | Caused by chronic conditions (e.g., hypertension, diabetes) |
| Management Approach | Requires emergency treatment (e.g., intravenous medications) | Managed with long-term medications and lifestyle changes |
| Hospitalization | Frequently requires hospitalization for stabilization | May require hospitalization during acute decompensation episodes |
| Prognosis | Variable; higher risk of mortality if untreated | Generally better prognosis but can lead to severe complications |
Pathophysiology
Acute Heart Failure Pathophysiology
Acute heart failure often results from a sudden event that affects the heart’s ability to pump blood effectively. Common causes include:
Myocardial infarction: Damage to the heart muscle due to a blockage in coronary arteries.
Acute valve dysfunction: Sudden problems with heart valves can lead to significant hemodynamic changes.
Arrhythmias: Rapid or irregular heartbeats can compromise cardiac output.
Infections: Conditions such as myocarditis can impair cardiac function acutely.
The pathophysiological changes involve increased filling pressures in the heart chambers, leading to pulmonary congestion and systemic fluid retention. This results in symptoms such as dyspnea, edema, and fatigue.
Chronic Heart Failure Pathophysiology
Chronic heart failure develops through a series of progressive changes in cardiac structure and function. The underlying mechanisms often include:
Left ventricular hypertrophy: Thickening of the heart muscle due to chronic pressure overload (e.g., hypertension).
Dilation of cardiac chambers: The chambers may enlarge as they try to accommodate increased blood volume.
Neurohormonal activation: Compensatory mechanisms involving hormones like norepinephrine and renin-angiotensin contribute to fluid retention and increased vascular resistance.
Chronic structural changes lead to a gradual decline in cardiac output, resulting in persistent symptoms that may fluctuate with episodes of decompensation.
Diagnosis
Diagnosing both types of heart failure involves a comprehensive clinical evaluation that includes:
Patient History: Assessing symptom onset, duration, severity, and any precipitating factors.
Physical Examination: Checking for signs such as edema, jugular venous distension, and abnormal lung sounds.
Diagnostic Tests:
Electrocardiogram (ECG): To identify arrhythmias or ischemic changes.
Echocardiography: To evaluate cardiac structure and function (ejection fraction).
Chest X-ray: To assess for pulmonary congestion or cardiomegaly.
Blood Tests: Including B-type natriuretic peptide (BNP) levels which can help differentiate between types of heart failure.
Treatment Strategies
Treatment for Acute Heart Failure
Management of acute heart failure focuses on immediate stabilization and symptom relief:
Oxygen Therapy: To improve oxygenation in patients experiencing respiratory distress.
Diuretics: Administered intravenously to reduce fluid overload quickly.
Vasodilators: Medications that help decrease cardiac workload by dilating blood vessels.
Inotropic Agents: May be used in cases where cardiac output needs enhancement.
Patients are often hospitalized for close monitoring and treatment adjustments based on their response.
Treatment for Chronic Heart Failure
Long-term management strategies for chronic heart failure aim at improving quality of life and preventing exacerbations:
Medications:
ACE Inhibitors/ARBs: To reduce afterload and improve survival rates.
Beta-blockers: To manage heart rate and improve myocardial function.
Diuretics: For ongoing management of fluid retention.
Aldosterone Antagonists: To mitigate fluid overload effects.
Lifestyle Modifications:
Dietary changes including sodium restriction.
Regular physical activity tailored to individual capacity.
Weight management strategies.
Monitoring for Decompensation Episodes:
Patients are educated about recognizing early signs of worsening symptoms that may require prompt medical attention.
Conclusion
Acute and chronic heart failure represent two distinct entities within the spectrum of cardiovascular disease. While both conditions share common symptoms such as shortness of breath and fatigue, their differences lie primarily in their onset, duration, severity, underlying causes, diagnostic approaches, and treatment strategies.
Related topics: