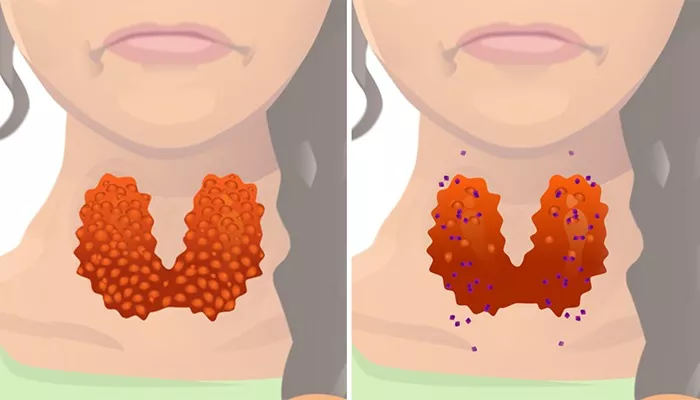
Hyperthyroidism is a condition characterized by an overproduction of thyroid hormones, which can significantly impact various bodily functions, including heart health. The thyroid gland, located at the front of the neck, plays a crucial role in regulating metabolism and energy levels through the secretion of hormones such as thyroxine (T4) and triiodothyronine (T3). When these hormones are produced in excess, they can lead to a range of cardiovascular complications, including heart failure. This article explores how hyperthyroidism contributes to heart failure, detailing the mechanisms involved and the implications for patient care.
Mechanisms by Which Hyperthyroidism Causes Heart Failure
The relationship between hyperthyroidism and heart failure is complex and multifaceted. Below are the primary mechanisms through which hyperthyroidism can lead to heart failure:
Increased Cardiac Output: Hyperthyroidism stimulates the heart to pump more blood than normal. This increased cardiac output can initially seem beneficial; however, over time, it places excessive strain on the heart muscle. The heart works harder to meet the body’s heightened demands for oxygen and nutrients due to elevated metabolism caused by excess thyroid hormones.
Tachycardia: One of the hallmark symptoms of hyperthyroidism is tachycardia, or an abnormally fast heartbeat. This rapid heart rate can lead to decreased filling time for the heart chambers, particularly during diastole (the phase when the heart relaxes). As a result, the heart may not fill adequately with blood before pumping it out again, leading to reduced cardiac efficiency and potential heart failure.
Atrial Fibrillation: Hyperthyroidism is associated with an increased risk of atrial fibrillation (AF), a condition characterized by irregular and often rapid heartbeats. AF can further exacerbate heart failure by reducing the effectiveness of blood flow from the atria to the ventricles, leading to inefficient pumping action and increased risk of thromboembolic events.
Increased Myocardial Oxygen Demand: The heightened activity level associated with hyperthyroidism increases myocardial oxygen demand. If coronary arteries are narrowed or blocked due to atherosclerosis, this increased demand can lead to angina (chest pain) or even myocardial infarction (heart attack), which can compromise cardiac function and lead to heart failure.
Hemodynamic Changes: Hyperthyroidism induces several hemodynamic changes that affect cardiovascular dynamics.
These changes include increased systolic blood pressure due to enhanced contractility and decreased diastolic pressure as blood vessels relax.
Such alterations can lead to left ventricular hypertrophy (enlargement) over time, which may contribute to diastolic dysfunction—a key factor in developing heart failure.
Direct Myocardial Toxicity: Excessive thyroid hormones can have direct toxic effects on cardiac myocytes (heart muscle cells). This toxicity may result in altered myocyte energy production and impaired contractile function, leading to a specific form of cardiomyopathy known as thyrotoxic cardiomyopathy. In severe cases, this can progress to dilated cardiomyopathy, characterized by ventricular dilation and impaired systolic function.
Fluid Retention: Hyperthyroidism can also cause fluid retention due to increased renal blood flow and glomerular filtration rate (GFR). This fluid overload can exacerbate symptoms of heart failure by increasing venous return (the amount of blood returning to the heart), leading to pulmonary congestion and peripheral edema.
Electrolyte Imbalances: Thyroid hormones influence electrolyte balance in the body. Hyperthyroidism may lead to imbalances in potassium and calcium levels, which are critical for proper cardiac function. Such imbalances can predispose individuals to arrhythmias and other cardiac complications that may contribute to heart failure.
Increased Catecholamine Levels: The hyperthyroid state often results in elevated levels of catecholamines (such as adrenaline), which increase heart rate and myocardial contractility but also raise the risk of arrhythmias. Chronic exposure to high catecholamine levels can lead to myocardial stress and eventual damage.
Clinical Implications
The interplay between hyperthyroidism and heart failure underscores the importance of early diagnosis and management of thyroid disorders in patients with cardiovascular disease. Effective treatment of hyperthyroidism can often reverse or mitigate its adverse effects on cardiac function.
Diagnosis: Clinicians should be vigilant in screening for thyroid dysfunction in patients presenting with symptoms of heart failure or arrhythmias. Blood tests measuring thyroid hormone levels (T3, T4) and thyroid-stimulating hormone (TSH) are essential for diagnosis.
Management Strategies: Treatment options for hyperthyroidism include antithyroid medications (such as methimazole), radioactive iodine therapy, or surgical intervention (thyroidectomy). Each treatment modality has its indications based on patient-specific factors such as age, comorbidities, and severity of hyperthyroid symptoms.
Cardiac Monitoring: Patients with hyperthyroidism should undergo regular cardiac evaluations, including echocardiography and electrocardiograms (ECGs), to assess cardiac function and detect any emerging complications like atrial fibrillation or left ventricular dysfunction.
Symptomatic Treatment: In cases where patients exhibit signs of heart failure, symptomatic management may include diuretics to reduce fluid overload, beta-blockers to control tachycardia and improve myocardial oxygen supply-demand balance, and other medications tailored to individual patient needs.
Patient Education: Educating patients about recognizing symptoms of worsening heart failure—such as shortness of breath, fatigue, swelling in extremities, or sudden weight gain—is crucial for timely intervention.
Conclusion
Hyperthyroidism poses significant risks for cardiovascular health, particularly through its association with heart failure.
Understanding the mechanisms by which excess thyroid hormones affect cardiac function is essential for healthcare providers managing patients with this condition. Timely diagnosis and appropriate treatment strategies can mitigate these risks, improve patient outcomes, and enhance quality of life for those affected by both hyperthyroidism and its cardiovascular complications.
In summary, while hyperthyroidism can lead to serious cardiac issues such as heart failure through various mechanisms—including increased cardiac output, tachycardia, atrial fibrillation, direct myocardial toxicity, fluid retention, electrolyte imbalances, increased catecholamines—effective management strategies exist that can help restore normal thyroid function and improve overall cardiac health.
Related topics: