Hypokalemia, defined as a serum potassium level of less than 3.5 mmol/L, is a common electrolyte disturbance that can have serious implications for cardiovascular health. Potassium is essential for various physiological functions, particularly in the heart, where it plays a crucial role in maintaining normal electrical activity and muscle contraction. When potassium levels drop significantly, the heart’s electrical system can become unstable, leading to arrhythmias—irregular heartbeats that can range from benign to life-threatening.
This article explores the relationship between hypokalemia and arrhythmias, detailing the underlying mechanisms and clinical implications. It will also discuss the causes of hypokalemia, its effects on cardiac function, and potential treatment strategies.
The Role of Potassium in Cardiac Function
Potassium is the most abundant intracellular cation and is vital for maintaining the resting membrane potential of cells, including cardiomyocytes (heart muscle cells). Normal potassium levels help regulate:
Action Potential: Potassium ions are crucial for repolarization during the cardiac action potential. This process allows the heart to reset after each beat.
Electrical Conductivity: Adequate potassium levels ensure proper conduction of electrical impulses through the heart’s conduction system.
Muscle Contraction: Potassium influences muscle contraction by affecting calcium handling within cardiac cells.
When potassium levels fall, several electrophysiological changes occur that predispose the heart to arrhythmias.
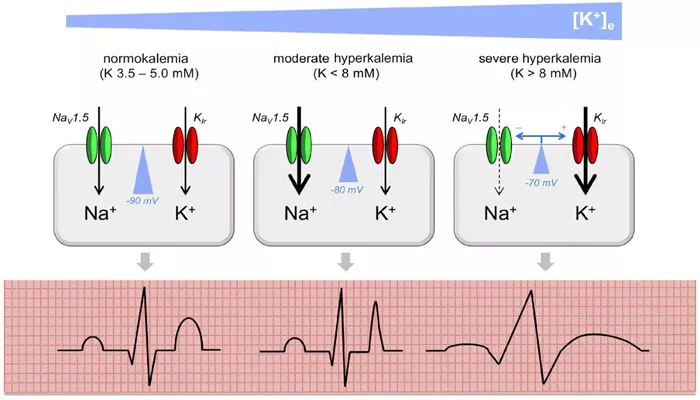
Mechanisms by Which Hypokalemia Causes Arrhythmias
Hypokalemia can lead to arrhythmias through several distinct mechanisms:
1. Altered Resting Membrane Potential
Low potassium levels increase the resting membrane potential, making it more positive (less negative). This change can lead to increased excitability of cardiac cells, which may trigger premature contractions or ectopic beats.
2. Prolonged Action Potential Duration
Hypokalemia prolongs the action potential duration and refractory period of cardiac cells. This prolonged duration increases the likelihood of reentrant circuits—pathways that allow electrical impulses to circulate continuously within the heart tissue, potentially leading to tachyarrhythmias such as atrial fibrillation or ventricular tachycardia.
3. Increased Automaticity
The decrease in potassium levels can enhance automaticity in cardiac pacemaker cells. This means that these cells may fire spontaneously without normal stimulus, contributing to arrhythmias such as atrial flutter or ventricular fibrillation.
4. Increased Threshold Potential
Hypokalemia raises the threshold potential required for depolarization. This alteration can lead to conditions where only a small stimulus can trigger an action potential, resulting in irregular heartbeats.
5. Decreased Conductivity
Low potassium levels reduce overall conductivity within cardiac tissues. This decrease can lead to slower conduction velocities and increased risk for reentrant arrhythmias.
6. Electrocardiographic Changes
Characteristic electrocardiographic (ECG) changes associated with hypokalemia include:
ST segment depression
T wave flattening or inversion
Prominent U waves
These ECG changes reflect altered repolarization dynamics and serve as important diagnostic markers for clinicians.
Clinical Manifestations of Arrhythmias Due to Hypokalemia
The types of arrhythmias that may occur due to hypokalemia include:
Premature Ventricular Contractions (PVCs): Early heartbeats originating from the ventricles.
Atrial Fibrillation: A rapid and irregular heartbeat that increases stroke risk.
Ventricular Tachycardia: A fast heart rate that can lead to more severe complications.
Torsade de Pointes: A specific type of polymorphic ventricular tachycardia often associated with prolonged QT intervals.
Ventricular Fibrillation: A life-threatening condition where the heart quivers instead of pumping effectively.
These arrhythmias can present with symptoms ranging from palpitations and dizziness to syncope (fainting) or sudden cardiac arrest in severe cases.
Causes of Hypokalemia
Understanding why hypokalemia occurs is essential for prevention and management. Common causes include:
Inadequate Dietary Intake: Insufficient consumption of potassium-rich foods such as fruits and vegetables.
Excessive Losses: Conditions leading to increased loss through urine or gastrointestinal tract, including:
- Diuretics use (especially loop and thiazide diuretics)
- Vomiting or diarrhea
- Excessive sweating
Hormonal Disorders: Conditions like hyperaldosteronism increase renal potassium excretion.
Medications: Certain medications can promote potassium loss or shift potassium into cells.
Chronic Illnesses: Conditions such as renal disease or metabolic disorders can disrupt potassium balance.
Diagnosis And Monitoring
Diagnosing hypokalemia typically involves measuring serum potassium levels through blood tests. Clinicians should also evaluate ECG findings for characteristic changes indicative of hypokalemia.
Continuous monitoring may be necessary for patients at high risk, especially those with existing cardiovascular conditions or those on diuretics.
Treatment Strategies
Treatment for hypokalemia focuses on restoring normal potassium levels and managing any underlying causes:
Potassium Supplementation:
Oral supplements are often sufficient for mild cases.
Intravenous potassium may be necessary for severe hypokalemia or when oral administration is not feasible.
Dietary Modifications:
Increasing intake of potassium-rich foods such as bananas, oranges, potatoes, spinach, and beans.
Medication Adjustments:
Reviewing medications that may contribute to potassium loss and considering alternatives if necessary.
Monitoring Electrolytes:
Regular monitoring of serum electrolytes in patients at risk to prevent recurrence.
Addressing Underlying Conditions:
Managing any hormonal imbalances or chronic illnesses contributing to hypokalemia.
Conclusion
Hypokalemia poses a significant risk for developing life-threatening arrhythmias due to its profound effects on cardiac electrophysiology. By understanding the mechanisms through which low potassium levels disrupt normal heart function, healthcare providers can better diagnose, treat, and prevent complications associated with this condition.
Related topics: