Coronary heart disease (CHD) is a leading cause of morbidity and mortality worldwide. It is primarily characterized by the narrowing or blockage of coronary arteries due to atherosclerosis, which can lead to heart attacks and other cardiovascular complications. While traditional risk factors such as high cholesterol, hypertension, and smoking are well-established contributors to CHD, the impact of environmental factors on cardiovascular health is gaining increasing attention in the medical community. This article explores how various environmental elements—ranging from air pollution to socioeconomic status—affect the incidence and progression of coronary heart disease.
The Role of Air Pollution
Air Quality and Cardiovascular Health
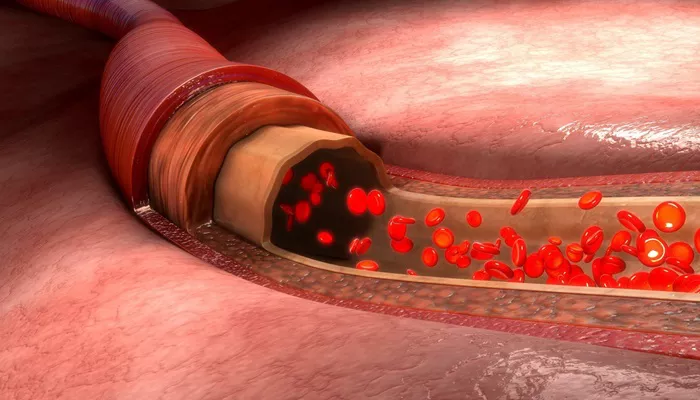
Air pollution is a significant environmental risk factor for CHD. Numerous studies have demonstrated a strong correlation between exposure to particulate matter (PM), nitrogen dioxide (NO2), and other pollutants with increased cardiovascular morbidity and mortality. Fine particulate matter (PM2.5) can penetrate deep into the lungs and enter systemic circulation, leading to systemic inflammation, oxidative stress, and endothelial dysfunction—all of which are critical pathways in the development of atherosclerosis.
Mechanisms of Action
The mechanisms by which air pollution contributes to CHD include:
Inflammation: Exposure to air pollutants can trigger inflammatory responses in the body, promoting the development of atherosclerotic plaques.
Oxidative Stress: Pollutants can increase oxidative stress, damaging endothelial cells and facilitating plaque formation.
Autonomic Nervous System Dysregulation: Air pollution exposure has been linked to changes in heart rate variability, which can increase the risk of arrhythmias and other cardiovascular events.
Research indicates that individuals living in urban areas with high levels of air pollution are at a greater risk for developing coronary heart disease compared to those in cleaner environments.
Socioeconomic Factors
Economic Disparities and Health Outcomes
Socioeconomic status (SES) plays a critical role in health outcomes, including the prevalence of coronary heart disease.
Individuals with lower SES often have limited access to healthcare, nutritious food, and opportunities for physical activity.
They may also experience higher levels of stress due to financial instability or unsafe living conditions.
Impact on Lifestyle Choices
Lower SES is associated with lifestyle factors that contribute to CHD:
Diet: Individuals with lower income may rely on cheaper, processed foods that are high in sugars and unhealthy fats.
Physical Activity: Lack of safe spaces for exercise can hinder physical activity levels among lower-income populations.
Healthcare Access: Limited access to preventive healthcare services can result in delayed diagnosis and treatment of risk factors like hypertension and diabetes.
Studies have shown that these socioeconomic disparities contribute significantly to the burden of coronary heart disease among disadvantaged populations.
Built Environment
Urban Design and Physical Activity
The built environment—comprising urban planning, transportation systems, and community resources—has a profound impact on physical activity levels. Walkable neighborhoods with access to parks and recreational facilities encourage physical activity, which is protective against CHD. Conversely, urban areas designed around car travel often discourage walking or cycling, contributing to sedentary lifestyles.
Green Spaces and Mental Health
Access to green spaces not only promotes physical activity but also has mental health benefits that indirectly affect cardiovascular health. Exposure to nature has been shown to reduce stress levels, improve mood, and enhance overall well-being. Chronic stress is a known risk factor for coronary heart disease; therefore, environments that promote relaxation and physical activity can mitigate some risks associated with CHD.
Climate Change
Increasing Cardiovascular Risks
Climate change poses a growing threat to public health, including cardiovascular health. Extreme weather events such as heatwaves can exacerbate existing health conditions, including those related to heart disease. Additionally, climate change is likely to increase air pollution levels due to higher temperatures facilitating the formation of ground-level ozone.
Vulnerable Populations
Certain populations are more vulnerable to the effects of climate change on cardiovascular health:
Elderly Individuals: Older adults are at greater risk for heat-related illnesses.
Low-Income Communities: These communities may lack resources for cooling during heatwaves or have pre-existing health disparities that exacerbate risks.
Research suggests that addressing climate change through policy interventions could significantly reduce the incidence of coronary heart disease by improving air quality and promoting healthier lifestyles.
Occupational Hazards
Workplace Environment
Occupational exposures are another environmental factor influencing coronary heart disease risk. Jobs that involve high levels of stress, long hours, or exposure to harmful substances can increase cardiovascular risk. For instance:
Chronic Stress: High-stress jobs can lead to unhealthy coping mechanisms such as smoking or poor dietary choices.
Exposure to Toxins: Certain occupations expose workers to chemicals or pollutants that may contribute directly or indirectly to cardiovascular diseases.
Employers play a crucial role in creating healthier work environments through wellness programs that promote physical activity and healthy eating.
Nutrition And Food Environment
Access to Healthy Foods
The availability of healthy food options in one’s environment significantly impacts dietary habits. Food deserts—areas with limited access to affordable and nutritious food—are often found in low-income neighborhoods. This lack of access contributes to poor dietary choices that elevate the risk for coronary heart disease.
Nutritional Education
Education about nutrition is vital for making informed food choices. Communities that provide resources for nutritional education can empower individuals to choose healthier options that support cardiovascular health. Programs aimed at improving food literacy can help mitigate some risks associated with poor dietary habits.
Conclusion
The interplay between environmental factors and coronary heart disease is complex but critical for understanding how we can reduce the burden of this condition. Addressing air pollution, socioeconomic disparities, built environment design, climate change impacts, occupational hazards, and nutritional access are essential components in preventing coronary heart disease.
Related topics: