Cardiomyopathy is a serious condition that affects the heart muscle, impairing its ability to pump blood effectively. This disease can lead to heart failure and other complications, making it a significant public health concern. Understanding the causes of cardiomyopathy is crucial for prevention, early detection, and management of the condition. While some cases of cardiomyopathy are idiopathic—meaning the cause is unknown—numerous factors have been identified that can contribute to the development of this disease. This article will explore the various causes of cardiomyopathy, categorizing them into genetic, acquired, and lifestyle-related factors.
Genetic Causes
Heredity and Genetic Mutations
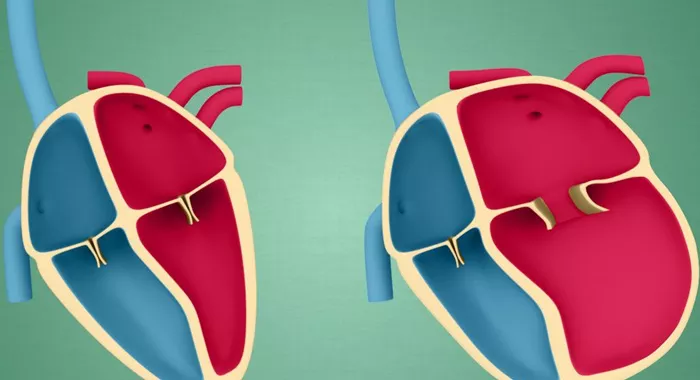
Genetic predisposition plays a substantial role in the development of certain types of cardiomyopathy. Family history is a significant risk factor; individuals with relatives who have cardiomyopathy or related heart conditions are more likely to develop the disease themselves. Hypertrophic cardiomyopathy (HCM), for instance, is often inherited in an autosomal dominant pattern, meaning only one copy of the mutated gene from an affected parent can lead to the condition in offspring.
Specific genetic mutations have been linked to various forms of cardiomyopathy. For example, mutations in genes responsible for cardiac muscle proteins can lead to familial dilated cardiomyopathy (DCM) and HCM. These genetic factors can disrupt normal heart muscle function, leading to structural changes and impaired pumping ability.
Congenital Heart Defects
Some individuals are born with structural abnormalities in their hearts that can predispose them to cardiomyopathy later in life. Congenital heart defects may affect the heart’s ability to pump blood efficiently or lead to other complications that contribute to the development of cardiomyopathy.
Acquired Causes
Coronary Artery Disease
Coronary artery disease (CAD) is one of the most common causes of acquired cardiomyopathy. CAD occurs when the coronary arteries become narrowed or blocked due to plaque buildup, reducing blood flow to the heart muscle. This lack of oxygen-rich blood can weaken the heart muscle over time, leading to ischemic cardiomyopathy.
Heart attacks, which result from severe CAD, can also cause damage to the heart muscle. The extent of damage can determine whether a person develops dilated cardiomyopathy as a result of their heart attack.
High Blood Pressure
Chronic high blood pressure (hypertension) is another significant risk factor for developing cardiomyopathy. When the heart has to work harder than normal to pump blood against elevated pressure in the arteries, it can lead to changes in heart muscle structure and function.
Over time, this increased workload may result in hypertrophy (thickening) of the heart muscle or dilation (enlargement), both of which are forms of cardiomyopathy.
Infections
Viral infections are recognized as a major cause of myocarditis, which can lead to dilated cardiomyopathy. Viruses such as Coxsackievirus B, adenovirus, and even COVID-19 have been implicated in causing inflammation of the heart muscle.
Inflammation can damage cardiac tissue and disrupt normal electrical signaling within the heart, potentially leading to arrhythmias and further complications.
Endocrine Disorders
Certain endocrine disorders can contribute to the development of cardiomyopathy. Conditions such as diabetes mellitus and thyroid disease can adversely affect heart function. For instance, uncontrolled diabetes may lead to metabolic changes that damage blood vessels and nerves supplying the heart58. Similarly, thyroid hormone imbalances—whether hyperthyroidism or hypothyroidism—can significantly impact cardiac function and structure.
Toxic Exposure
Exposure to toxins can also be a contributing factor in acquired cardiomyopathy. Long-term alcohol abuse is a well-known cause; excessive alcohol consumption can lead to alcoholic cardiomyopathy due to its toxic effects on cardiac cells.
Additionally, recreational drugs such as cocaine and certain medications used in chemotherapy can cause damage to the heart muscle.
Lifestyle Factors
Obesity
Obesity is associated with various health issues, including cardiovascular diseases. Excess body weight increases the risk for hypertension and diabetes—two significant contributors to cardiomyopathy. Furthermore, obesity may directly affect cardiac structure by promoting inflammation and metabolic syndrome.
Sedentary Lifestyle
A lack of physical activity contributes not only to obesity but also directly affects cardiovascular health. Regular exercise strengthens the heart muscle and improves circulation; conversely, inactivity can lead to deconditioning of cardiac function over time.
Dietary Factors
Poor dietary choices can also play a role in developing conditions that lead to cardiomyopathy. Diets high in saturated fats, sugars, and sodium contribute to obesity and hypertension. A lack of essential nutrients—such as vitamins B1 (thiamine) and D—can also impair heart health and increase susceptibility to cardiomyopathy.
Other Contributing Factors
Pregnancy-Related Cardiomyopathy
Peripartum cardiomyopathy is a rare form that occurs during late pregnancy or shortly after childbirth. The exact cause remains unclear but may involve hormonal changes and increased stress on the cardiovascular system during pregnancy.
Autoimmune Diseases
Autoimmune disorders such as rheumatoid arthritis or lupus may also contribute to cardiomyopathy through chronic inflammation that affects cardiac tissues. These conditions can lead to myocarditis or other forms of cardiac dysfunction.
Conclusion
Understanding the causes of cardiomyopathy is essential for effective prevention and management strategies. Genetic factors play a crucial role in some cases, particularly with inherited forms like hypertrophic cardiomyopathy. Acquired causes such as coronary artery disease, high blood pressure, infections, endocrine disorders, toxic exposure, obesity, sedentary lifestyle choices, and poor dietary habits significantly contribute to this serious condition.
In summary, while some causes of cardiomyopathy remain elusive or idiopathic, many identifiable risk factors highlight opportunities for preventive measures that could ultimately reduce morbidity associated with this debilitating condition.
Related topics: