Coronary ischemia, also known as myocardial ischemia, is a condition where the heart muscle doesn’t receive enough oxygenated blood to function properly. This reduction in blood flow can lead to chest pain, shortness of breath, and in severe cases, heart attacks. Understanding the causes of coronary ischemia is crucial for prevention, early diagnosis, and effective treatment. In this article, we will explore the various factors that contribute to coronary ischemia, breaking them down into understandable sections.
Introduction to Coronary Ischemia
Coronary ischemia occurs when the blood supply to the heart muscle is reduced or blocked, usually due to problems with the coronary arteries. These arteries are responsible for delivering oxygen-rich blood to the heart. If the blood flow is restricted, the heart muscle may become oxygen-starved, leading to a variety of symptoms. Over time, persistent coronary ischemia can damage the heart tissue, weakening the heart’s ability to pump blood effectively.
Several factors can cause coronary ischemia, with the most common being atherosclerosis, a condition where plaque builds up inside the arteries. However, other factors, such as blood clots, arterial spasms, or an increased demand for oxygen by the heart muscle, can also contribute to this condition. Let’s take a closer look at the main causes of coronary ischemia.
1. Atherosclerosis: The Leading Cause of Coronary Ischemia
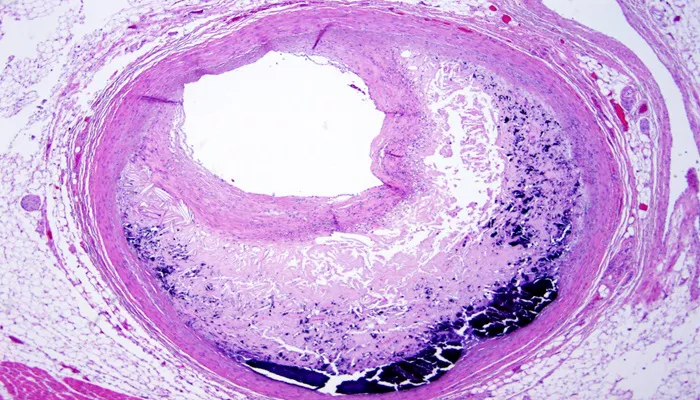
Atherosclerosis is the primary cause of coronary ischemia. This condition involves the buildup of fatty deposits, cholesterol, and other substances on the walls of the coronary arteries. Over time, this plaque can harden and narrow the arteries, restricting blood flow. The accumulation of plaque is gradual, often taking decades, and may not produce noticeable symptoms until the narrowing of the arteries becomes severe.
How Atherosclerosis Develops
Atherosclerosis begins when the inner lining of the artery is damaged by factors such as high blood pressure, high cholesterol, smoking, or diabetes. This damage allows fatty substances to accumulate in the artery walls. Over time, this leads to plaque formation, which narrows and stiffens the arteries. In some cases, the plaque may rupture, leading to the formation of a blood clot, further obstructing the blood flow.
The Impact of Atherosclerosis on Coronary Ischemia
As the coronary arteries become narrowed due to atherosclerosis, the heart muscle receives less oxygenated blood. This insufficient blood flow can result in chest pain (angina), especially during physical exertion when the heart’s oxygen demand increases. If the plaque ruptures and a blood clot forms, it can completely block the artery, leading to a heart attack.
2. Blood Clots: A Sudden Cause of Coronary Ischemia
Blood clots can form within the coronary arteries, either at the site of a ruptured plaque or in the absence of pre-existing plaque. When a blood clot completely blocks an artery, the heart muscle can become deprived of oxygen, resulting in coronary ischemia. This is often the most acute and dangerous form of ischemia, as it can lead to a heart attack (myocardial infarction) within minutes.
How Blood Clots Cause Ischemia
The process begins when a plaque inside the artery ruptures, exposing its contents to the bloodstream. This triggers the blood’s clotting response, causing platelets to aggregate and form a clot at the site of rupture. If the clot is large enough to block the flow of blood through the coronary artery, ischemia occurs. This blockage can lead to the death of heart tissue if not quickly treated.
Risk Factors for Blood Clots
Several factors can increase the likelihood of blood clot formation, including:
- High cholesterol
- Smoking
- Diabetes
- High blood pressure
- Sedentary lifestyle
- Certain medications (such as birth control pills or hormone replacement therapy)
3. Coronary Artery Spasm: A Temporary Cause of Ischemia
A coronary artery spasm occurs when a segment of a coronary artery temporarily tightens or narrows, reducing blood flow to the heart muscle. This spasm can last for several minutes and can be caused by various factors, including stress, drug use, or cold exposure. While coronary artery spasms are usually temporary, they can still cause significant chest pain and discomfort.
How Coronary Artery Spasms Cause Ischemia
During a coronary artery spasm, the smooth muscle in the artery wall constricts, causing the artery to narrow. This reduces the blood flow to the heart, leading to ischemia. Spasms may occur even in the absence of atherosclerosis and are often linked to conditions like angina, particularly “Prinzmetal’s angina,” which is caused by these spasms.
Risk Factors for Coronary Artery Spasm
Common triggers for coronary artery spasms include:
- Smoking
- Cocaine or other drug use
- Excessive alcohol consumption
- Stress or anxiety
- Exposure to cold weather
- Certain medications
4. Increased Oxygen Demand: A Demand-Supply Imbalance
Coronary ischemia can also occur when the heart muscle’s oxygen demand exceeds the supply of blood and oxygen. This imbalance can happen during periods of intense physical activity, emotional stress, or when the heart is working harder than usual.
Conditions That Increase Oxygen Demand
Several factors can increase the heart’s oxygen demand, including:
Physical exertion: Exercise increases the heart’s need for oxygenated blood.
Emotional stress: Anxiety, anger, or stress can elevate heart rate and blood pressure, increasing oxygen consumption.
Fever or infection: A higher body temperature causes the heart to beat faster and demand more oxygen.
Anemia: Reduced red blood cells lead to less oxygen being transported to the tissues, making the heart work harder.
In these situations, if the coronary arteries are already narrowed (due to atherosclerosis), the increased demand for oxygen may not be met, leading to ischemia.
5. Other Contributing Factors to Coronary Ischemia
While the causes mentioned above are the most common, there are several other risk factors and conditions that can contribute to coronary ischemia:
High Blood Pressure (Hypertension)
Chronic high blood pressure can damage the walls of the coronary arteries, leading to atherosclerosis and narrowing of the arteries. Additionally, the heart has to work harder to pump blood against the higher pressure, which increases oxygen demand.
Diabetes
Diabetes can accelerate the process of atherosclerosis by increasing the level of blood sugar, which in turn causes damage to the blood vessels. Over time, this can lead to narrowing of the coronary arteries, contributing to ischemia.
Smoking
Cigarette smoking is a major risk factor for coronary ischemia. The chemicals in tobacco smoke can damage blood vessels, increase blood pressure, and promote the formation of plaque in the arteries.
High Cholesterol
Excessive cholesterol in the blood, particularly low-density lipoprotein (LDL), can contribute to the formation of plaque in the arteries. This plaque buildup can narrow the coronary arteries and reduce blood flow to the heart muscle.
Conclusion
Coronary ischemia is a serious condition that can lead to severe complications, including heart attacks. The primary causes of ischemia include atherosclerosis, blood clots, coronary artery spasms, and an increased demand for oxygen. However, a variety of risk factors—such as high blood pressure, diabetes, smoking, and high cholesterol—can exacerbate the condition.
Related topics:
- How Does the Environment Affect Coronary Heart Disease
- What Is Occlusive Coronary Arteriosclerosis?
- How Long Can You Live with Heart Valve Disease