Hyperlipidemia, or high cholesterol, is a common and serious condition that can significantly increase the risk of cardiovascular diseases, including heart attack, stroke, and coronary artery disease. The prevalence of hyperlipidemia is alarmingly high, and it often goes undiagnosed because it does not present noticeable symptoms until significant damage has already occurred. Screening for hyperlipidemia is essential for early detection and prevention, but when exactly should screening begin? The timing of lipid screening depends on several factors, including age, risk factors, and the presence of underlying health conditions.
In this article, we will explore the guidelines for screening for hyperlipidemia, explain the factors that influence the timing of screenings, and provide a clearer understanding of when individuals should begin to have their cholesterol levels tested.
What Is Hyperlipidemia?
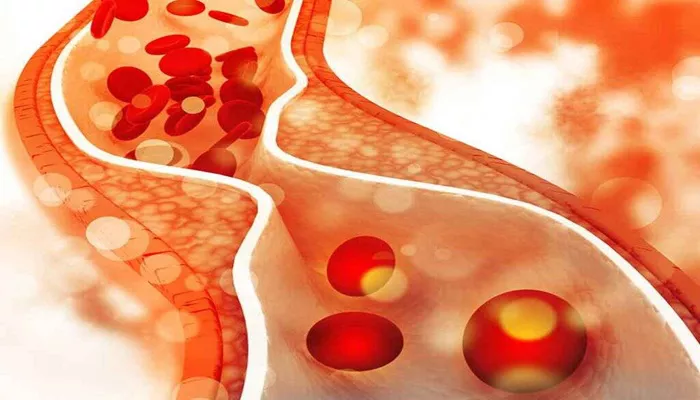
Before we delve into the specifics of screening, it is important to understand what hyperlipidemia is. Hyperlipidemia refers to abnormally high levels of lipids (fats) in the blood. The primary components measured during a lipid panel are:
Total Cholesterol: The overall amount of cholesterol in the blood.
Low-Density Lipoprotein (LDL): Often referred to as “bad cholesterol,” which can build up in the walls of arteries and increase the risk of heart disease.
High-Density Lipoprotein (HDL): Known as “good cholesterol,” which helps remove LDL from the bloodstream.
Triglycerides: A type of fat found in the blood that can also increase the risk of heart disease when levels are high.
Elevated LDL cholesterol and high triglycerides are the main contributors to hyperlipidemia, both of which can lead to the development of atherosclerosis, a condition where fatty deposits build up in the arteries and restrict blood flow.
Risk Factors for Hyperlipidemia
Certain factors can increase the likelihood of developing hyperlipidemia. These include:
Family history of heart disease or high cholesterol: Genetics play a major role in cholesterol levels, with some individuals inheriting genes that predispose them to high cholesterol.
Age: Cholesterol levels tend to rise with age, particularly in men after 45 and in women after menopause.
Gender: Men are more likely to have high cholesterol at younger ages, while women’s cholesterol levels rise after menopause.
Unhealthy diet: A diet high in saturated fats, trans fats, and cholesterol can raise LDL levels and contribute to hyperlipidemia.
Physical inactivity: Lack of exercise can lower HDL cholesterol and contribute to weight gain, further increasing lipid levels.
Obesity: Being overweight or obese often leads to higher levels of triglycerides and LDL, and lower levels of HDL.
Other health conditions: Conditions such as diabetes, hypothyroidism, and kidney disease can lead to increased cholesterol levels.
When to Start Screening for Hyperlipidemia
The timing of cholesterol screening is critical for identifying hyperlipidemia before it leads to severe cardiovascular events. Below, we will break down the recommendations for when cholesterol screening should start, based on various age groups and risk profiles.
1. Children and Adolescents (Ages 9-11)
For children, the American Academy of Pediatrics (AAP) recommends that lipid screening should begin at age 9 to 11 years for those with risk factors for hyperlipidemia, including a family history of early heart disease, high cholesterol, or obesity.
Screening is typically done once during this age range and may be repeated if there are concerns or changes in health status.
For children without a family history of hyperlipidemia or cardiovascular disease and who do not have other risk factors, screening is generally not recommended unless other health conditions arise.
2. Adults (Ages 20-39)
The American College of Cardiology (ACC) and the American Heart Association (AHA) recommend that adults should begin routine screening for hyperlipidemia starting at age 20. This screening is generally done every 4-6 years, depending on risk factors.
For adults in this age group with known risk factors—such as obesity, smoking, diabetes, or a family history of early heart disease—more frequent screening may be necessary. Lifestyle changes, including adopting a heart-healthy diet and increasing physical activity, are encouraged to help manage cholesterol levels.
3. Adults (Ages 40-75)
For adults between the ages of 40 and 75, the guidelines are more specific. The ACC/AHA recommends assessing the risk for cardiovascular disease (CVD) using the Pooled Cohort Risk Assessment Equations. These risk calculators consider factors like cholesterol levels, blood pressure, smoking status, diabetes, and age to estimate the 10-year risk of developing CVD.
If a person’s risk is calculated to be moderate to high, cholesterol screening becomes critical, and treatment options, including statin therapy, may be considered to reduce the risk of heart disease. If a person is found to be at low risk, regular screenings every 4-6 years may be sufficient.
4. Older Adults (Ages 75 and Above)
For adults aged 75 and older, the decision to screen for hyperlipidemia should be individualized, based on overall health, life expectancy, and existing cardiovascular risk factors. Routine screening may not be necessary for healthy individuals, but those with risk factors for cardiovascular disease or a history of high cholesterol should continue to be monitored.
In many cases, treatment goals shift from simply lowering cholesterol to improving overall cardiovascular health, particularly in patients who have existing heart disease.
Key Guidelines for Screening
The following general guidelines should be considered when determining when and how to screen for hyperlipidemia:
Routine screening should begin at age 20 for individuals with average risk and continue every 4-6 years.
Early screening (ages 9-11) is recommended for children with risk factors, such as family history or obesity.
High-risk individuals (those with diabetes, hypertension, or a family history of heart disease) should begin screening earlier and more frequently, as determined by a healthcare provider.
Risk assessment using calculators like the Pooled Cohort Risk Equations should be done for individuals aged 40-75 to assess the need for treatment and more frequent cholesterol testing.
How Often Should You Be Screened?
Once you start screening, the frequency depends on your risk level:
Low-risk adults: Screening every 4-6 years is usually adequate.
High-risk adults: Those with high cholesterol, diabetes, or other cardiovascular risk factors should be screened more often (e.g., every 1-2 years).
Individuals on lipid-lowering treatment: Those receiving treatment for high cholesterol should be monitored regularly (every 3-6 months) to assess the effectiveness of the therapy.
Why Screening Matters
Early detection of hyperlipidemia is crucial because it allows for lifestyle modifications and, in some cases, medication to lower cholesterol levels before significant damage to the arteries occurs. For those at high risk of cardiovascular disease, managing cholesterol early can prevent heart attacks, strokes, and other severe complications. Regular screening is an opportunity to catch abnormal cholesterol levels before they become problematic.
Conclusion
Screening for hyperlipidemia is essential for preventing heart disease, particularly for those at increased risk. The timing of screenings varies based on age, risk factors, and family history. For children with risk factors, screening should begin as early as age 9. For adults, regular screenings should start at age 20 and continue every 4-6 years, depending on risk factors.
Individuals at high risk should begin screenings earlier and more frequently. By detecting hyperlipidemia early, we can take preventive measures to reduce the likelihood of heart disease and improve overall cardiovascular health.
Related topics: