Coronary spasm, also known as vasospasm, is a temporary constriction or narrowing of the coronary arteries—the blood vessels that supply the heart muscle with oxygen-rich blood. This spasm can cause chest pain, and in some cases, it may lead to more severe complications like heart attacks. Understanding the symptoms and sensations associated with coronary spasm can be crucial for early identification and timely intervention.
This article will explore what a coronary spasm feels like, how it affects the body, and what individuals should know about its causes and potential treatments. The goal is to provide a comprehensive yet clear explanation of this condition for both patients and those interested in learning more about heart health.
What Is A Coronary Spasm?
Before diving into the symptoms, it is important to understand what a coronary spasm is. In a coronary spasm, the smooth muscle inside the coronary arteries constricts, restricting blood flow. This spasm can occur suddenly and may last for seconds or minutes. During this time, the heart muscle is deprived of oxygen, which can lead to chest pain (angina) or other more severe symptoms. While coronary spasms are temporary, they can result in significant discomfort and, if left untreated, may lead to heart attacks or arrhythmias.
Unlike atherosclerosis (plaque build-up in the arteries), which is a more chronic condition, coronary spasm occurs suddenly and unpredictably. This makes it difficult to identify in advance, and its symptoms often resemble other heart-related conditions.
How Does A Coronary Spasm Feel?
The sensations that come with a coronary spasm vary from person to person, but they generally involve sudden, intense chest pain. The key characteristics of the pain and the symptoms associated with coronary spasm include:
1. Chest Pain or Tightness
The most common symptom of a coronary spasm is chest pain or discomfort. This pain often comes on suddenly and may feel like a heavy weight or tightness in the chest. The pain can be severe, and it may radiate to other areas, such as the arms, neck, jaw, or back. The discomfort can resemble the pain experienced during a heart attack, though it usually resolves after a short period.
The pain associated with a coronary spasm is typically:
Sharp or squeezing: You may feel as though something is pressing tightly against your chest.
Intense but short-lasting: The pain can come on quickly and may last anywhere from a few seconds to several minutes.
Intermittent: In some cases, the spasm may cause multiple episodes of pain over a few hours or even days.
2. Pain Radiating to Other Parts of the Body
While chest pain is the most common symptom, coronary spasms may also cause discomfort that radiates to other areas of the body. This can include:
Left arm: The left arm, especially the forearm or hand, is a common site for pain to radiate during a coronary spasm.
Neck, jaw, or back: The pain may travel to the neck, jaw, or upper back.
This is similar to the radiating pain seen in heart attacks, which can sometimes make it difficult to distinguish between the two conditions without further testing.
Upper stomach: Some individuals may experience pain or discomfort in the upper abdominal area, which can be mistaken for indigestion or heartburn.
3. Shortness of Breath
Because the heart muscle is temporarily deprived of oxygen during a coronary spasm, many individuals experience shortness of breath.
This sensation can occur along with chest pain or as a result of the body struggling to compensate for the lack of oxygen.
Shortness of breath can be particularly alarming if it occurs suddenly and without any apparent cause.
4. Dizziness or Lightheadedness
In some cases, a coronary spasm may lead to a feeling of dizziness or lightheadedness. This is due to the heart’s reduced ability to pump blood effectively, which lowers oxygen levels in the body. If the spasm is severe or prolonged, the decreased blood flow can cause fainting or near-fainting sensations.
5. Palpitations
Some people may experience palpitations during a coronary spasm. Palpitations are the sensation of your heart beating irregularly or more rapidly than usual. This can happen because the coronary spasm disrupts the normal rhythm of the heart, leading to arrhythmias.
Factors That Can Trigger Coronary Spasm
Coronary spasms can occur without warning, but certain factors may increase the likelihood of experiencing one. These include:
1. Stress
Physical or emotional stress is one of the most common triggers for coronary spasms. Stress causes the release of hormones such as adrenaline, which can affect the smooth muscles in the coronary arteries, potentially leading to a spasm.
2. Cold Weather
Exposure to cold temperatures can trigger a coronary spasm. The body constricts blood vessels in response to cold, and this can affect the coronary arteries, causing them to narrow and restrict blood flow.
3. Smoking
Nicotine and other chemicals in cigarettes can cause the blood vessels to constrict, which increases the risk of coronary spasms. Smoking is also a significant risk factor for heart disease, which can exacerbate the effects of coronary spasms.
4. Drug Use
Certain drugs, particularly cocaine and other stimulants, can trigger coronary spasms. These substances stimulate the sympathetic nervous system, which can cause blood vessels to constrict and lead to spasms in the coronary arteries.
5. High Blood Pressure
Chronic hypertension can damage the walls of the arteries, making them more susceptible to spasms. Elevated blood pressure can also cause the heart to work harder, increasing the risk of spasm.
When Should You Seek Medical Attention?
If you experience chest pain or discomfort that is sudden and severe, it is important to seek medical attention immediately.
Although a coronary spasm may resolve on its own, the symptoms are similar to those of a heart attack, and it is important to rule out more serious conditions.
If you experience any of the following, you should seek urgent medical help:
Sudden, severe chest pain that lasts more than a few minutes.
Pain that radiates to the arms, neck, jaw, or back.
Difficulty breathing or shortness of breath.
Dizziness or fainting.
A history of heart disease or coronary artery disease.
Diagnosis And Treatment of Coronary Spasms
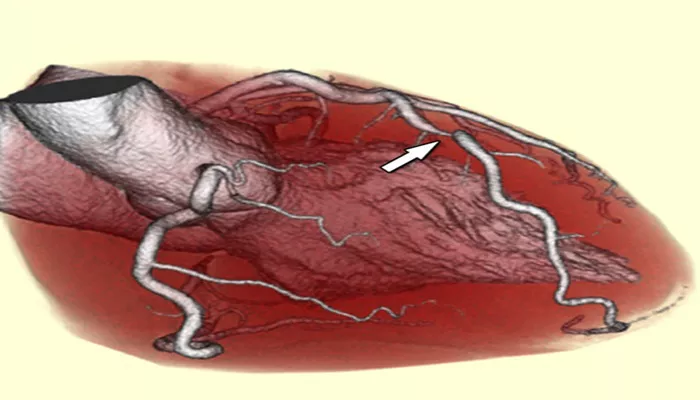
To diagnose a coronary spasm, doctors will typically take a detailed medical history, conduct a physical exam, and order tests such as an electrocardiogram (ECG), stress tests, or coronary angiography. These tests help rule out other heart conditions and confirm the presence of a coronary spasm.
Treatment for coronary spasms usually involves medications that help relax the coronary arteries and prevent further spasms. These medications can include:
Calcium channel blockers: These drugs help relax the muscles in the blood vessels, which can prevent spasms.
Nitrates: Nitrates are medications that dilate blood vessels and can help relieve chest pain caused by coronary spasms.
Statins: Statins may be prescribed if there is evidence of plaque buildup in the arteries, as they can help prevent future spasms by lowering cholesterol levels.
In addition to medication, lifestyle changes such as quitting smoking, managing stress, and avoiding cold temperatures or drug use can help prevent coronary spasms.
Conclusion
A coronary spasm can be an alarming and painful experience. The sudden chest pain, shortness of breath, dizziness, and other symptoms can be distressing, especially if they mimic a heart attack. However, with timely diagnosis and treatment, coronary spasms can often be managed effectively. It is important for individuals to understand the signs of coronary spasm and seek medical help if they experience any concerning symptoms.
Related topics:
- What Causes Coronary Ischemia?
- How Does the Environment Affect Coronary Heart Disease
- What Is Occlusive Coronary Arteriosclerosis?