Hyperlipidemia, or high blood cholesterol, is a condition that significantly increases the risk of cardiovascular diseases, including heart attacks, strokes, and atherosclerosis. Since lipid levels can fluctuate due to various factors, monitoring them is essential for managing the condition and preventing long-term health complications. Understanding the optimal frequency of monitoring, as well as the factors that affect lipid levels, is critical for both healthcare providers and patients.
This article will delve into the importance of monitoring hyperlipidemia, the ideal frequency for testing, and the factors that influence lipid levels.
What Is Hyperlipidemia?
Hyperlipidemia refers to an abnormally high concentration of lipids (fats) in the blood, including cholesterol and triglycerides. The most common form is elevated levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol. Another lipid of concern is high triglyceride levels, which are associated with an increased risk of heart disease and pancreatitis.
Cholesterol is essential for the body, as it is involved in producing hormones, vitamin D, and bile acids that help digest fat.
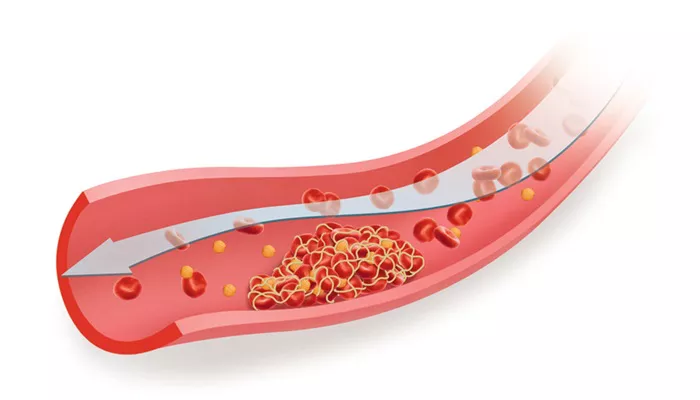
However, too much cholesterol, particularly LDL cholesterol, can accumulate in the arteries, leading to the development of plaque. This plaque buildup narrows and hardens the arteries, a condition called atherosclerosis, which increases the risk of heart attacks and strokes.
Types of Lipids Involved in Hyperlipidemia
Low-Density Lipoprotein (LDL): Often called “bad” cholesterol, LDL carries cholesterol to cells throughout the body.
Excessive LDL can lead to plaque buildup in the arteries.
High-Density Lipoprotein (HDL): Known as “good” cholesterol, HDL helps remove excess cholesterol from the bloodstream and transports it to the liver for excretion.
Triglycerides: These are the most common type of fat found in the blood. Elevated triglyceride levels can contribute to heart disease and are commonly seen in individuals with obesity, diabetes, and metabolic syndrome.
Why Is Monitoring Hyperlipidemia Important?
Monitoring hyperlipidemia is crucial for several reasons:
Early Detection of Risk Factors: Elevated cholesterol levels often have no immediate symptoms. Regular monitoring helps detect abnormal lipid levels before they lead to serious cardiovascular conditions.
Personalized Treatment Plans: The frequency of monitoring helps healthcare providers determine the effectiveness of treatment plans, such as lifestyle changes or medications like statins, in managing lipid levels.
Risk Stratification: Regular testing allows for assessing the overall risk of cardiovascular disease, including heart attacks and strokes. This helps to implement preventive measures or adjust current treatments.
Preventing Complications: High cholesterol levels are closely linked to the development of heart disease, liver problems, and other complications. Frequent monitoring can help avoid these outcomes through timely interventions.
How Often Should You Monitor Hyperlipidemia?
The frequency of hyperlipidemia monitoring depends on several factors, including the patient’s age, overall health, risk factors, and whether they are undergoing treatment. Generally, the following guidelines apply:
1. For Adults with No Risk Factors
For adults who are considered low-risk (i.e., no history of heart disease, diabetes, or other cardiovascular conditions), the American Heart Association (AHA) recommends that adults aged 20 and older should have their lipid levels checked at least once every four to six years. This is usually done through a fasting lipid profile test, which measures total cholesterol, LDL, HDL, and triglycerides.
2. For Adults with High Risk or Established Cardiovascular Disease
Patients who are at high risk for cardiovascular diseases or who already have a history of conditions like heart disease, stroke, or peripheral artery disease should have their cholesterol levels monitored more frequently. The following guidelines apply:
Every 3-6 months: Patients on lipid-lowering medications like statins, or those who have had a cardiovascular event, should monitor their lipid levels more often. Testing every three to six months helps assess whether the treatment plan is effective and allows adjustments if necessary.
More frequently in case of significant changes: If a patient’s cholesterol levels fluctuate drastically, or if their health changes (such as weight loss, medication changes, or the development of other health conditions), more frequent monitoring may be required.
3. For Individuals with Diabetes
People with diabetes are at an increased risk of cardiovascular disease, and managing hyperlipidemia is a key component of their care. The American Diabetes Association recommends lipid screening at least once a year for individuals with diabetes. If cholesterol levels are abnormal, more frequent testing may be needed to monitor the effectiveness of lifestyle changes or medications.
4. For Patients Starting or Adjusting Lipid-Lowering Medications
When a patient starts taking lipid-lowering medications, such as statins, fibrates, or PCSK9 inhibitors, it is important to monitor their lipid levels within the first 4-12 weeks to ensure the medication is working effectively and to check for any potential side effects. After this initial period, lipid levels should be monitored every 3-6 months to track progress and adjust medication dosages as needed.
Factors That Influence The Frequency of Monitoring
The frequency of monitoring hyperlipidemia varies depending on several factors:
1. Age
Young Adults (20-39 years): Routine screening for hyperlipidemia is not necessary unless the individual has risk factors such as obesity, a family history of heart disease, or diabetes.
Middle-Aged Adults (40-59 years): Regular lipid checks become more important at this age, especially if the individual has risk factors for cardiovascular disease.
Older Adults (60+ years): Older adults are at a higher risk of developing hyperlipidemia and cardiovascular diseases. More frequent monitoring may be necessary for those with elevated cholesterol levels or who are already on treatment.
2. Family History
A family history of heart disease, hyperlipidemia, or early death due to cardiovascular issues increases the need for more frequent monitoring. Individuals with a first-degree relative (parent or sibling) who developed heart disease at an early age (before 55 for men or 65 for women) may need more frequent screening, especially if other risk factors are present.
3. Lifestyle Factors
Obesity: Obese individuals are at a higher risk of developing hyperlipidemia. Regular monitoring is essential to track lipid levels and ensure that lifestyle interventions are effective.
Diet: A diet high in saturated fats and low in fruits and vegetables can contribute to elevated cholesterol levels. Regular monitoring is recommended for individuals with poor dietary habits.
Physical Activity: Lack of physical activity can lead to elevated cholesterol levels. Individuals who are inactive should have their cholesterol levels checked more frequently.
4. Other Health Conditions
Hypertension: Individuals with high blood pressure are at increased risk of cardiovascular disease, making regular lipid screening crucial.
Metabolic Syndrome: A group of conditions, including high blood pressure, high blood sugar, excess fat around the waist, and abnormal cholesterol levels, increases the risk of heart disease and should prompt more frequent lipid testing.
Conclusion
The frequency of monitoring hyperlipidemia depends on the patient’s individual health profile and risk factors. While adults with no significant risk factors may only need screening every four to six years, those with diabetes, heart disease, or high cholesterol require more frequent testing. Lifestyle factors, age, family history, and other health conditions can all influence how often lipid levels should be checked. Regular monitoring, combined with appropriate treatment and lifestyle modifications, plays a critical role in preventing the complications of hyperlipidemia and improving overall cardiovascular health.
Related topics: