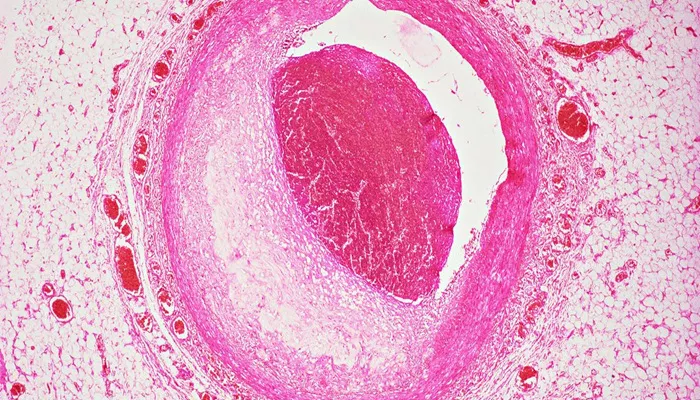
Coronary artery calcification (CAC) refers to the buildup of calcium deposits in the walls of the coronary arteries, which are responsible for supplying oxygenated blood to the heart. These arteries can become hardened over time as calcium accumulates, a condition often associated with atherosclerosis (hardening of the arteries). Severe coronary artery calcification means that the level of calcium deposition in the coronary arteries has reached a stage where it may significantly impair blood flow, increasing the risk of heart disease, heart attack, or other serious cardiovascular conditions.
This article delves into the meaning of severe coronary artery calcification, its causes, symptoms, diagnosis, and treatment options.
What Is Coronary Artery Calcification?
The coronary arteries are responsible for providing oxygen and nutrients to the heart muscle. Over time, certain risk factors can cause the walls of these arteries to become thickened and hardened. One of the major contributors to this process is the accumulation of calcium, which becomes embedded within the artery walls. This condition is called coronary artery calcification. It can be seen in both early and late stages of atherosclerosis.
Coronary artery calcification is considered an indicator of the presence and severity of coronary artery disease (CAD). The extent of calcification can be measured through imaging techniques like computed tomography (CT) scans or coronary calcium scoring. When this calcification becomes severe, it often leads to narrowing or stiffening of the arteries, reducing blood flow and potentially leading to dangerous cardiovascular events.
Causes of Severe Coronary Artery Calcification
Several factors can contribute to the development of severe coronary artery calcification. Understanding these factors is crucial for both prevention and treatment.
1. Aging
As individuals age, the risk of developing coronary artery calcification increases. Over time, the walls of the arteries can become more susceptible to damage, allowing for the buildup of calcium and plaque.
This process typically begins after the age of 40 and accelerates as individuals get older.
2. High Cholesterol Levels
Elevated cholesterol, particularly low-density lipoprotein (LDL) cholesterol, is one of the primary causes of plaque formation within the arteries. Over time, this plaque can become calcified. When plaque in the arteries becomes calcified, it hardens, making it more difficult for the arteries to expand and contract, which impedes normal blood flow.
3. Hypertension (High Blood Pressure)
High blood pressure can damage the inner lining of the arteries, making them more prone to the deposition of calcium and other substances. As the artery walls thicken and stiffen due to the increased pressure, calcium builds up, leading to coronary artery calcification. In combination with other risk factors like cholesterol, hypertension can significantly worsen the condition.
4. Smoking
Cigarette smoke contains harmful chemicals that damage the blood vessels. These substances can cause inflammation and oxidative stress, which contribute to the formation of plaque in the coronary arteries. This plaque can eventually become calcified, resulting in coronary artery calcification.
5. Diabetes
Diabetes, particularly uncontrolled diabetes, can accelerate the process of arterial calcification. High blood sugar levels contribute to the thickening of blood vessels and increase the risk of plaque buildup. Over time, the calcification of these plaques can lead to severe narrowing of the coronary arteries.
6. Inflammation
Chronic inflammation in the body, which can be caused by conditions such as autoimmune diseases or persistent infections, plays a key role in the development of atherosclerosis and coronary artery calcification. Inflammation contributes to the accumulation of fatty deposits in the arteries, and as these deposits mature, they may become calcified.
7. Genetics
Family history plays a crucial role in determining an individual’s risk for coronary artery calcification. If a person has a parent or sibling with heart disease or other related conditions, their risk of developing coronary artery calcification is increased. Genetic factors can also influence how the body responds to lifestyle factors such as diet, exercise, and stress.
8. Obesity
Excess body fat, particularly visceral fat (fat around the organs), is strongly associated with coronary artery disease and calcification. Obesity leads to higher levels of inflammation, insulin resistance, and an increased risk of hypertension and high cholesterol, all of which contribute to the development of coronary artery calcification.
9. Lack of Physical Activity
A sedentary lifestyle is another significant risk factor for coronary artery calcification. Regular physical activity helps to maintain healthy blood pressure, cholesterol levels, and weight, which can reduce the risk of calcification in the coronary arteries. Lack of exercise, on the other hand, promotes conditions like obesity and hypertension, which are major contributors to the buildup of calcium in the arteries.
10. Dietary Factors
An unhealthy diet, particularly one high in saturated fats, trans fats, and cholesterol, can contribute to the development of atherosclerosis and coronary artery calcification. Diets that lack essential nutrients like omega-3 fatty acids and antioxidants can exacerbate inflammation and promote plaque buildup. Additionally, excessive consumption of processed foods and sugary drinks can lead to obesity and diabetes, both of which increase the risk of coronary artery calcification.
Symptoms of Severe Coronary Artery Calcification
Severe coronary artery calcification itself may not present any obvious symptoms. In fact, many individuals with significant coronary artery calcification do not experience symptoms until the condition has advanced. However, as calcification leads to the narrowing of the coronary arteries, symptoms may include:
Chest Pain (Angina): Reduced blood flow to the heart muscle due to narrowed arteries can lead to chest pain, especially during physical activity or stress.
Shortness of Breath: As the heart struggles to pump blood efficiently, individuals may experience difficulty breathing, particularly during exertion.
Fatigue: Chronic fatigue can result from the heart’s inability to supply enough oxygen-rich blood to the body.
Heart Attack: In severe cases, coronary artery calcification can lead to the rupture of atherosclerotic plaques, which may trigger a heart attack (myocardial infarction).
Arrhythmias: The heart’s electrical system may be affected by reduced blood flow, leading to abnormal heart rhythms.
Diagnosis of Severe Coronary Artery Calcification
The diagnosis of coronary artery calcification is typically made through imaging techniques. Some of the most common diagnostic tools include:
1. Coronary Artery Calcium (CAC) Scoring
This is the most widely used method for assessing the severity of coronary artery calcification. A CT scan of the heart is used to measure the amount of calcium in the coronary arteries. The results are then given a score, with higher scores indicating more extensive calcification and a greater risk of heart disease.
2. CT Angiography
This imaging technique uses a CT scan combined with contrast dye to provide detailed images of the coronary arteries. It helps in visualizing the extent of coronary artery disease and calcification.
3. X-Ray
In some cases, an X-ray may be used to detect significant calcium buildup in the arteries. However, this is less detailed than a CT scan and is typically not the first choice for diagnosis.
Treatment of Severe Coronary Artery Calcification
While coronary artery calcification cannot be reversed, several treatment options can help manage the condition and reduce the risk of heart attacks or other complications. Treatment may include lifestyle changes, medications, and in some cases, surgical interventions.
1. Lifestyle Modifications
Diet: A heart-healthy diet rich in fruits, vegetables, whole grains, and healthy fats can help reduce cholesterol levels and inflammation.
Exercise: Regular physical activity helps improve cardiovascular health by lowering blood pressure, reducing cholesterol, and maintaining a healthy weight.
Smoking Cessation: Quitting smoking is one of the most important steps in preventing further damage to the arteries.
Stress Management: Reducing stress through techniques like meditation, yoga, or deep breathing can lower the risk of cardiovascular events.
2. Medications
Statins: These drugs help lower cholesterol levels and reduce the risk of plaque buildup in the arteries.
Aspirin: Low-dose aspirin may be recommended to reduce the risk of blood clots, which can form on calcified plaques and block blood flow.
Blood Pressure Medications: Medications such as ACE inhibitors, beta-blockers, or diuretics may be prescribed to control high blood pressure.
3. Surgical Interventions
Angioplasty and Stenting: In cases where severe calcification leads to significant artery blockage, a procedure called angioplasty may be used to open up the artery. A stent (a small mesh tube) may be inserted to keep the artery open.
Coronary Artery Bypass Surgery (CABG): In cases of extensive coronary artery disease, bypass surgery may be required to reroute blood flow around blocked or calcified arteries.
Conclusion
Severe coronary artery calcification is a serious condition that can lead to significant heart disease and increase the risk of heart attacks. It is caused by a combination of aging, lifestyle factors, and underlying health conditions like high cholesterol, hypertension, and diabetes. While it may not always show symptoms until it becomes severe, it is a key indicator of coronary artery disease. Early detection and management through lifestyle changes, medications, and, in some cases, surgical intervention can help reduce the risks associated with this condition and improve heart health.
Related topics: