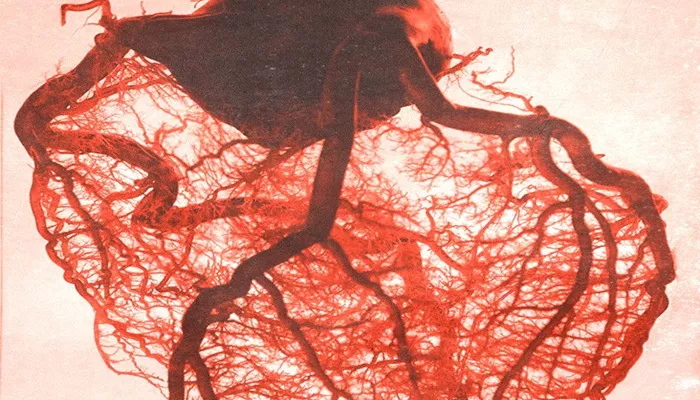
Coronary microvascular disease (MVD) is a condition affecting the tiny blood vessels that supply the heart muscle. Unlike traditional coronary artery disease, which involves the larger coronary arteries, coronary MVD specifically targets the microvessels. These small vessels play a crucial role in delivering oxygen and nutrients to the heart muscle. When they become damaged or narrowed, the heart may not receive adequate blood supply, which can lead to chest pain (angina) and other symptoms similar to those seen in more common forms of heart disease.
One of the most important questions for patients diagnosed with coronary MVD is whether the condition can be reversed.
This article will delve into the mechanisms behind coronary MVD, the potential for reversing or managing the disease, and current treatments that can improve outcomes for affected individuals.
What Is Coronary Microvascular Disease?
Coronary MVD refers to dysfunction or damage to the small coronary arteries that supply blood to the heart muscle. These vessels are typically less than 500 microns in diameter and cannot be seen or treated easily through traditional diagnostic tools like coronary angiograms. The condition is more difficult to diagnose because it doesn’t show up on standard imaging tests.
In coronary MVD, the blood vessels may become stiff or narrowed, reducing blood flow and limiting the heart muscle’s ability to function properly. As a result, patients may experience chest pain, fatigue, or shortness of breath, often during physical activity or times of stress.
The Causes of Coronary Microvascular Disease
Several factors contribute to the development of coronary MVD. Some of the most common causes include:
Atherosclerosis: Fatty deposits can accumulate in the microvessels, just as they do in larger arteries. This process, known as atherosclerosis, can lead to vessel narrowing and impaired blood flow.
Inflammation: Chronic inflammation is another factor that may damage the small coronary vessels. Conditions such as diabetes, hypertension, and autoimmune diseases can increase inflammation in the blood vessels.
Spasm of Microvessels: Microvessels may go into spasm, reducing blood flow even in the absence of physical blockage.
This can be triggered by stress, certain medications, or other external factors.
Genetics: Genetic predispositions may play a role in the development of coronary MVD. A family history of heart disease can increase the likelihood of developing this condition.
Hormonal Changes: Some research suggests that hormonal changes, particularly those associated with menopause, may contribute to the onset of coronary MVD in women.
Can Coronary Microvascular Disease Be Reversed?
At present, coronary microvascular disease cannot be fully reversed in the traditional sense. However, there are several approaches to managing and even improving the condition, reducing symptoms, and preventing further damage. The idea of “reversal” may be better understood as the potential for halting progression, reducing the severity of symptoms, and improving heart function.
Current Approaches to Managing Coronary MVD
1. Lifestyle Modifications
The first line of defense against coronary MVD involves addressing modifiable risk factors that contribute to the disease’s progression.
These lifestyle changes may not reverse the condition entirely, but they can significantly improve heart health and reduce the likelihood of complications:
Healthy Diet: Eating a diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce inflammation and prevent further damage to the coronary microvessels. Avoiding high-fat, high-sugar foods is crucial for managing risk factors such as obesity and high cholesterol.
Physical Activity: Regular exercise strengthens the heart and improves circulation. It can help reduce blood pressure, lower cholesterol levels, and promote overall cardiovascular health. Aerobic exercise, such as walking, jogging, or swimming, is particularly beneficial.
Stress Management: Since stress can exacerbate microvascular dysfunction, adopting stress-reduction techniques such as meditation, yoga, or deep breathing exercises can help improve symptoms.
Smoking Cessation: Smoking is a major risk factor for cardiovascular disease and can damage blood vessels. Quitting smoking is essential for improving heart health and reducing further complications.
2. Pharmacological Interventions
Though coronary MVD cannot be completely reversed with medication, various drugs can help manage the condition and alleviate symptoms.
These treatments may include:
Nitroglycerin and Nitrates: These medications can help dilate the blood vessels, improving blood flow to the heart muscle and alleviating chest pain.
Beta-Blockers: Beta-blockers reduce the heart’s workload by slowing the heart rate and lowering blood pressure. These can be helpful in reducing symptoms of coronary MVD, such as angina.
Calcium Channel Blockers: Calcium channel blockers help relax and dilate the blood vessels, which can improve blood flow in cases of microvascular spasm.
ACE Inhibitors: Angiotensin-converting enzyme (ACE) inhibitors can help manage high blood pressure and reduce the strain on the heart.
Statins: Statins, which are typically used to lower cholesterol levels, may also help reduce inflammation in the arteries, including the microvessels.
Antiplatelet Medications: These drugs, such as aspirin, can help prevent blood clot formation and reduce the risk of a heart attack.
3. Interventional Procedures
While coronary MVD is often resistant to traditional interventions like stenting or bypass surgery, some advanced techniques may help improve blood flow in specific cases:
Microvascular Intervention: In some cases, specialized procedures such as percutaneous coronary interventions (PCI) may be used to improve blood flow, but these are not as effective in microvessels as they are in larger arteries.
Coronary Flow Reserve (CFR) Measurement: This procedure helps assess how well blood is flowing through the coronary microvessels, which can help guide treatment decisions. While it does not directly reverse MVD, it can provide valuable information on how well the microvessels are functioning.
4. Emerging Therapies
Several promising therapies are being researched to improve outcomes for patients with coronary MVD:
Gene Therapy: Some studies are exploring the possibility of using gene therapy to regenerate damaged microvessels or improve blood flow in these small vessels.
Stem Cell Therapy: Stem cell treatments are under investigation for their potential to repair or regenerate damaged blood vessels. Though still in early stages, these therapies hold promise for future treatments.
Angiogenesis: This process, which involves the growth of new blood vessels, could potentially help bypass damaged microvessels. Research is ongoing to determine if angiogenesis can be stimulated in coronary MVD patients.
The Role of Early Diagnosis
Early diagnosis of coronary MVD is essential for managing the condition before it leads to more severe complications like heart failure. Since coronary MVD is often asymptomatic or difficult to detect, it is crucial to monitor individuals at high risk, including those with a family history of heart disease, diabetes, or high blood pressure.
Advanced imaging techniques, such as coronary magnetic resonance imaging (MRI) or positron emission tomography (PET) scans, are now being used to detect coronary microvascular dysfunction more effectively than traditional angiograms.
These methods can help physicians assess the condition of the microvessels and tailor treatment accordingly.
Conclusion
Although coronary microvascular disease cannot be fully reversed, significant strides can be made in managing the condition, reducing symptoms, and improving heart health. By addressing modifiable risk factors, adopting a healthy lifestyle, and utilizing pharmacological and interventional therapies, individuals with coronary MVD can experience improved quality of life and better long-term outcomes.
Related topics: