Coronary artery disease (CAD) is one of the most common heart-related health issues around the world. It happens when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of fatty deposits called plaque. This blockage can restrict blood flow, leading to chest pain (angina), shortness of breath, and in some cases, heart attacks.
One of the most common treatments for this condition is the insertion of coronary stents. These small, mesh-like tubes are designed to keep the coronary arteries open and ensure proper blood flow to the heart muscle. However, many patients and healthcare providers have concerns about how long these stents last, their effectiveness, and the potential need for further treatment.
In this article, we will explore the longevity of coronary stents, the factors that can influence their lifespan, and what patients need to know about maintaining their heart health after stent implantation.
What Is A Coronary Stent?
Before we dive into how long coronary stents last, it is important to understand what a stent is and how it works.
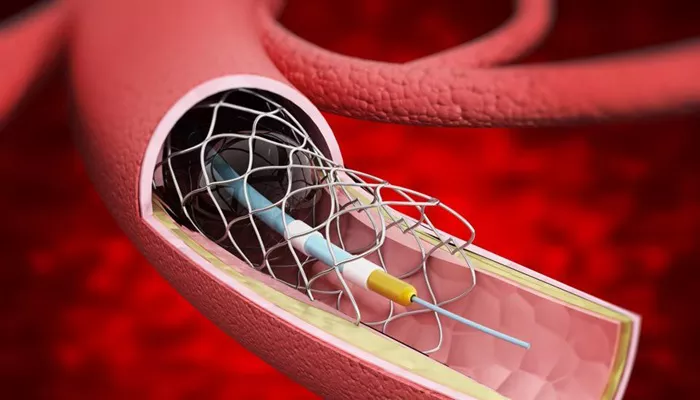
A coronary stent is a small, tube-shaped device made from metal or plastic that is inserted into a coronary artery to prevent it from becoming narrowed or blocked. The stent is usually placed during a procedure called angioplasty, in which a balloon is inflated inside the artery to open up the blockage, and the stent is then deployed to keep the artery open.
Stents can be categorized into two main types:
Bare-metal stents (BMS): These are made of metal and do not contain any medication. While they are effective at keeping arteries open, there is a risk that scar tissue may form inside the stent, leading to re-narrowing (restenosis).
Drug-eluting stents (DES): These stents are coated with medication that helps to prevent the formation of scar tissue. As a result, drug-eluting stents have a lower risk of restenosis compared to bare-metal stents.
Both types of stents help improve blood flow and reduce symptoms related to CAD, such as chest pain. However, they work in slightly different ways, and their longevity can vary.
How Long Do Coronary Stents Last?
The lifespan of a coronary stent is often the subject of many questions from patients. In general, coronary stents are designed to last a lifetime. However, there are a few nuances that need to be addressed to better understand this answer.
Immediate Effects of a Stent: Once a stent is implanted, it is meant to stay in place permanently. The stent will continue to hold the artery open, ensuring proper blood flow to the heart muscle. In most cases, the stent itself does not “wear out” or “expire.” However, the artery itself may continue to experience changes over time that can affect how well the stent performs.
Restenosis and Re-blockage: One of the biggest concerns with coronary stents, particularly with bare-metal stents, is the possibility of restenosis. This occurs when scar tissue forms inside the stent, causing the artery to become narrowed again.
The risk of restenosis is highest in the first six months following the procedure. After that, the risk of further narrowing decreases significantly.
Drug-eluting stents (DES), on the other hand, are coated with medication that helps to prevent the formation of this scar tissue. As a result, restenosis is much less common in patients with DES, but it is still possible, especially if the patient does not follow a healthy lifestyle or adhere to prescribed medications (e.g., blood thinners or antiplatelet drugs).
Factors Affecting Stent Longevity:
Medication Adherence: Patients who do not follow their doctor’s instructions regarding medications, such as antiplatelet drugs (like aspirin and clopidogrel), are at greater risk of developing complications after stent placement. Not taking these medications as prescribed can increase the risk of blood clots forming in or around the stent, potentially leading to blockage.
Lifestyle Factors: Uncontrolled risk factors such as high blood pressure, high cholesterol, smoking, obesity, and a sedentary lifestyle can accelerate the development of new blockages in the arteries, including around the stent. Healthy lifestyle changes can help prevent these issues and increase the long-term success of stents.
Stent Type: As mentioned earlier, drug-eluting stents tend to have better long-term outcomes compared to bare-metal stents because they help reduce the risk of restenosis. Patients with drug-eluting stents generally experience longer-lasting results and a lower likelihood of needing additional interventions.
Long-Term Outcomes: Studies show that coronary stents can last many years when properly maintained. On average, patients with stents can expect to live for several decades without major issues, provided they follow their doctor’s guidance on medication, lifestyle changes, and follow-up care.
However, it is important to note that while the stent itself may last indefinitely, the health of the artery and the heart still need ongoing attention. Patients may need additional stents or treatments later in life if new blockages develop, but the first stent will continue to function as intended.
Signs of Stent Complications
Even though coronary stents are designed to last for many years, some patients may experience complications that could affect the stent’s function. Here are some signs and symptoms that may indicate an issue with the stent:
Chest pain (angina): This can be a sign that the artery has become narrowed again, or that the stent has become blocked.
Shortness of breath: Difficulty breathing may indicate reduced blood flow to the heart muscle, which could be caused by a blockage near the stent.
Fatigue or dizziness: These symptoms can occur if the heart is not receiving enough oxygen due to a blocked artery.
Heart attack symptoms: If a blood clot forms inside the stent, it could lead to a heart attack. Symptoms include severe chest pain, nausea, and sweating.
If you experience any of these symptoms, it is essential to seek medical help immediately.
Can A Stent Be Replaced?
In some cases, if a stent becomes blocked or develops complications, it may need to be replaced or treated with a procedure such as balloon angioplasty or another stent insertion. However, this is not common. The vast majority of patients with coronary stents will not require replacement and can expect their stents to function effectively for many years.
What Happens After A Stent Is Placed?
After having a coronary stent implanted, it is crucial to follow up with your cardiologist regularly. These visits typically involve:
Monitoring medication adherence: It is important to take prescribed medications, especially antiplatelet drugs, to reduce the risk of blood clots and restenosis.
Lifestyle modifications: Your doctor may recommend lifestyle changes to help manage risk factors such as high blood pressure, high cholesterol, and smoking.
Regular check-ups: Follow-up visits may include imaging tests (e.g., angiography) to ensure the stent is functioning properly and to check for any new blockages in the arteries.
Conclusion
Coronary stents are a vital tool in managing coronary artery disease and preventing heart attacks. While coronary stents do not have an expiration date and are designed to last a lifetime, their effectiveness can be influenced by several factors. Most importantly, maintaining a healthy lifestyle, taking prescribed medications, and adhering to follow-up care can significantly increase the long-term success of stent placement.
Related topics: