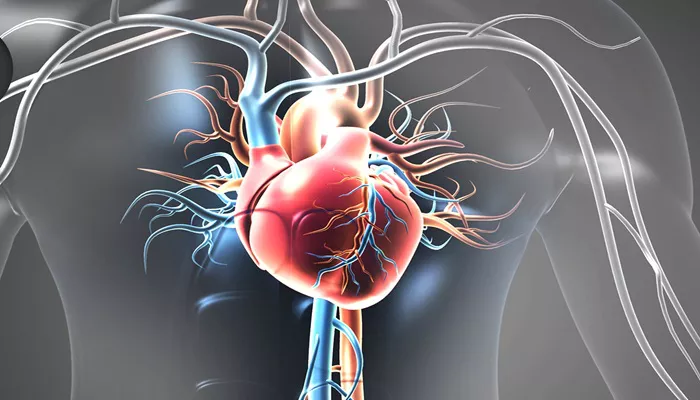
Heart failure (HF) is a complex and chronic condition that affects the heart’s ability to pump blood effectively, leading to a range of systemic complications. One such complication is the elevation of liver enzymes, a condition often seen in individuals with advanced or poorly controlled heart failure. The liver plays a crucial role in detoxifying the blood and metabolizing nutrients, and its function can be significantly impacted by circulatory problems related to heart failure.
In this article, we will explore the mechanisms that link heart failure to elevated liver enzymes, explain how this condition is diagnosed, and highlight the clinical significance of these enzyme elevations in heart failure patients.
Understanding Heart Failure And Its Impact on The Body
Heart failure occurs when the heart is unable to pump enough blood to meet the body’s demands. This condition can result from a variety of underlying causes, including coronary artery disease, high blood pressure, heart attacks, and valvular heart disease. Heart failure is categorized into two main types:
Left-sided heart failure: The left side of the heart cannot pump blood efficiently to the rest of the body, leading to fluid buildup in the lungs (pulmonary congestion).
Right-sided heart failure: The right side of the heart cannot pump blood to the lungs for oxygenation, causing fluid to accumulate in the abdomen, legs, and feet (peripheral edema).
When heart failure progresses, both sides of the heart can be affected, leading to congestive heart failure (CHF), which can have widespread consequences for the body’s organs and systems, including the liver.
The Liver And Its Role in The Body
The liver is a vital organ responsible for many important functions, including:
Metabolism: The liver breaks down nutrients from food and produces essential proteins, such as albumin and clotting factors.
Detoxification: It filters toxins and waste products from the bloodstream, including alcohol, medications, and metabolic byproducts.
Storage: The liver stores vitamins, minerals, and glycogen (a form of glucose used for energy).
Bile Production: The liver produces bile, which is essential for digesting fats.
The liver’s role in filtering and processing blood makes it highly susceptible to damage from poor circulation and low oxygen levels, which can occur in heart failure.
How Heart Failure Leads to Elevated Liver Enzymes
Elevated liver enzymes are often used as markers of liver injury or dysfunction. The primary liver enzymes measured in clinical practice are:
Alanine aminotransferase (ALT): This enzyme is found mainly in the liver and is released into the bloodstream when liver cells are damaged.
Aspartate aminotransferase (AST): AST is present in several tissues, including the liver, heart, and muscles. Like ALT, it is elevated when cells in these tissues are damaged.
Alkaline phosphatase (ALP): This enzyme is found in the liver, bones, kidneys, and bile ducts. Elevated ALP levels can suggest liver disease or bile duct obstruction.
Gamma-glutamyl transferase (GGT): GGT is elevated in the presence of liver disease, alcohol consumption, and bile duct obstruction.
There are several mechanisms by which heart failure can cause elevated liver enzymes:
1. Congestive Hepatopathy (Liver Congestion)
One of the most common causes of elevated liver enzymes in heart failure is congestive hepatopathy, which occurs when blood backs up in the liver due to poor blood flow from the heart. In right-sided heart failure, the heart is unable to pump blood effectively to the lungs, causing a rise in pressure in the right atrium and the veins that drain blood from the body.
This elevated venous pressure is transmitted to the liver through the hepatic veins, leading to congestion and poor perfusion.
When the liver becomes congested, its normal blood flow is compromised, which can lead to liver cell damage and the release of enzymes such as ALT, AST, and ALP into the bloodstream. The resulting condition is often referred to as “nutmeg liver” due to its characteristic appearance on imaging.
2. Hypoxia (Low Oxygen Levels)
In heart failure, particularly in severe or decompensated cases, the heart’s inability to pump blood effectively leads to poor tissue oxygenation, a condition known as hypoxia. The liver, being a highly metabolic organ, requires a constant supply of oxygen to function properly. When oxygen levels in the blood are low, liver cells can become damaged and release enzymes into the bloodstream.
The hypoxia-induced liver injury may worsen in patients with both right-sided and left-sided heart failure, as poor cardiac output leads to systemic hypoxia, affecting multiple organs, including the liver.
3. Elevated Systemic Pressures And Portal Hypertension
Another contributing factor to liver enzyme elevation in heart failure is the development of portal hypertension. The portal vein carries blood from the gastroi
ntestinal tract to the liver, and it is vulnerable to increased pressure when the right side of the heart is failing. This is because blood returning from the body must pass through the right heart, and when it cannot flow efficiently, it causes a backpressure effect on the veins, including the portal vein.
Increased pressure in the portal vein causes portal hypertension, which can lead to damage to the liver’s blood vessels and increase the risk of liver congestion, fibrosis, and eventual cirrhosis. This chronic stress on the liver may result in elevated liver enzymes as a reflection of ongoing liver injury.
4. Hepatic Fibrosis And Cirrhosis
Chronic congestion and hypoxia in the liver can lead to progressive liver damage over time. The liver responds to repeated injury by forming scar tissue in a process known as fibrosis. If fibrosis continues unchecked, it can lead to cirrhosis, which is the end stage of liver scarring.
Cirrhosis is associated with elevated liver enzymes, especially AST, ALT, and ALP, as liver function becomes increasingly impaired. In heart failure patients with longstanding liver congestion, cirrhosis can develop, which further exacerbates liver enzyme abnormalities.
5. Medication Effects
Many patients with heart failure are prescribed medications to manage their condition, including diuretics, ACE inhibitors, beta-blockers, and anticoagulants. While these medications are effective in controlling heart failure symptoms, some of them can have hepatotoxic effects, leading to elevated liver enzymes. For example:
Diuretics, which are commonly used to reduce fluid retention in heart failure, can cause electrolyte imbalances and affect liver function.
ACE inhibitors and angiotensin receptor blockers (ARBs) can sometimes lead to mild liver enzyme elevations.
Statins, commonly prescribed to control cholesterol in heart failure patients, may also lead to liver enzyme abnormalities, especially in those with pre-existing liver issues.
6. Systemic Inflammation and Cytokine Release
Heart failure is often accompanied by chronic inflammation, which can contribute to elevated liver enzymes. Inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α) and interleukins, are released during heart failure and can have a negative effect on liver function.
These cytokines promote hepatic cell injury and fibrosis, leading to the release of enzymes into the bloodstream.
Diagnosis And Monitoring of Elevated Liver Enzymes in Heart Failure
When elevated liver enzymes are detected in a patient with heart failure, it is important to evaluate the underlying cause and the degree of liver dysfunction. Some key diagnostic steps include:
Liver function tests: These include measurements of ALT, AST, ALP, and GGT, as well as other markers such as bilirubin and albumin.
Imaging: Ultrasound, CT scans, or MRIs can help identify liver congestion, cirrhosis, or other structural abnormalities.
Liver biopsy: In some cases, a liver biopsy may be necessary to assess the degree of fibrosis or cirrhosis.
Echocardiography: This is used to evaluate the heart’s function and identify any worsening heart failure or right-sided heart failure.
Conclusion
Elevated liver enzymes are a common finding in patients with heart failure, especially in those with right-sided heart failure or congestive heart failure. The mechanisms behind these elevations include liver congestion, hypoxia, portal hypertension, hepatic fibrosis, and medication-related liver injury. Monitoring liver enzymes in heart failure patients is crucial for detecting liver dysfunction early and preventing further complications.
Related topics: