Coronary artery dissection (CAD) is a rare but serious condition where there is a tear or separation in the inner layers of the coronary artery wall. This can lead to the formation of a blood clot or a decrease in blood flow to the heart muscle, potentially causing heart attacks or other cardiovascular complications. While coronary artery dissection is most often seen in patients with no significant risk factors for heart disease, it can also affect those with underlying conditions.
Understanding the causes, risk factors, and potential triggers of coronary artery dissection is essential for both patients and healthcare providers to effectively diagnose, manage, and treat this condition.
In this article, we will delve into the causes of coronary artery dissection, exploring both known and less understood factors.
We will also examine the signs, symptoms, and treatment options available to patients diagnosed with this potentially life-threatening disorder.
What Is Coronary Artery Dissection?
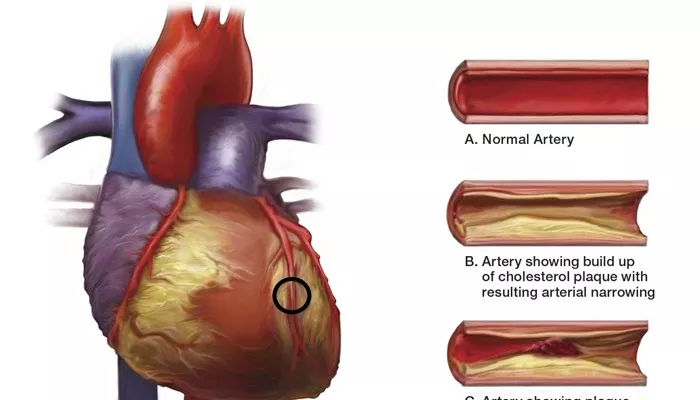
Before exploring the causes, it is important to understand what coronary artery dissection entails. The coronary arteries are responsible for supplying blood to the heart muscle. These arteries consist of three layers: the inner intima, the middle media, and the outer adventitia. A coronary artery dissection occurs when there is a tear in the intima, which can allow blood to enter the wall of the artery, creating a false lumen or channel. This tear can narrow or block the artery, reducing blood flow to the heart, leading to ischemia (lack of oxygen), and, in some cases, a heart attack.
Types of Coronary Artery Dissection
There are two main types of coronary artery dissection:
Spontaneous Coronary Artery Dissection (SCAD): This occurs without any obvious external cause. It is most common in women, particularly those who are middle-aged or pregnant, and can happen without any underlying coronary artery disease.
Traumatic Coronary Artery Dissection: This is typically caused by external injury to the artery, such as from a car accident or a medical procedure. This type is less common but can have significant consequences.
While SCAD is the focus of this article, both types of dissections can lead to serious cardiovascular events if not managed appropriately.
Causes of Coronary Artery Dissection
1. Spontaneous Coronary Artery Dissection (SCAD)
Spontaneous coronary artery dissection (SCAD) is still not fully understood, but several factors may increase the risk of developing this condition. These factors include genetic, hormonal, and vascular conditions.
Genetic Factors
Certain genetic conditions and familial predispositions may play a role in SCAD. For instance, individuals with Marfan syndrome, Ehlers-Danlos syndrome, or Loeys-Dietz syndrome, all of which involve connective tissue abnormalities, have a higher risk of developing coronary artery dissection. These conditions can make the blood vessels more prone to tears and dissections due to their structural weaknesses.
There may also be a hereditary component, as SCAD can sometimes run in families, though more research is needed to confirm specific genes involved in this condition.
Hormonal Influences
SCAD is more prevalent in women, particularly during or after pregnancy. It has been suggested that hormonal changes during pregnancy, particularly increased levels of estrogen, may affect the integrity of the blood vessels. Estrogen is known to have an effect on collagen production, and a decrease in collagen can make the artery walls more vulnerable to tearing.
Additionally, women who have recently given birth are at a higher risk for SCAD, suggesting that pregnancy-related stress on the cardiovascular system may contribute to arterial dissection.
Vascular Conditions
Some vascular conditions, such as fibromuscular dysplasia (FMD), are closely associated with SCAD. FMD is a disease that affects the walls of the arteries, causing abnormal growths or thickening that can lead to weakened vessel walls. This makes them more susceptible to tearing and dissection. Other conditions like high blood pressure (hypertension), cholesterol abnormalities, or coronary artery abnormalities can also contribute to the risk of SCAD.
2. Traumatic Coronary Artery Dissection
While spontaneous coronary artery dissection occurs without a clear trigger, traumatic dissection is often the result of external forces acting on the artery.
Trauma from Physical Injury
Traumatic coronary artery dissection can occur as a result of physical injury, such as in a car accident, a fall, or sports injuries. Blunt force trauma to the chest can damage the coronary arteries, leading to dissection. This type of dissection is typically associated with fractures or other serious injuries and often requires immediate medical intervention.
Medical Procedures and Interventions
Certain medical interventions, such as cardiac catheterization, angioplasty, or stent placement, can sometimes cause a tear in the coronary artery. The use of a catheter to insert a stent or perform angioplasty can cause injury to the artery wall, leading to a dissection. While these procedures are generally safe, the risk of dissection, though rare, increases with complicated or high-risk interventions.
3. Hypertension (High Blood Pressure)
High blood pressure is a major risk factor for many cardiovascular conditions, and it can contribute to coronary artery dissection as well.
The increased pressure in the blood vessels can cause damage to the arterial walls over time, weakening the vessel and making it more prone to dissection. In patients with uncontrolled hypertension, the risk of arterial tears and other complications is significantly higher.
4. Atherosclerosis and Plaque Build-Up
Although spontaneous coronary artery dissection typically occurs in individuals without significant coronary artery disease, those with atherosclerosis (plaque build-up) are at an increased risk. Plaque buildup can weaken the artery walls and contribute to the formation of tears. In some cases, the dissection may occur at the site of a pre-existing plaque, which can further exacerbate the condition by causing a blood clot or a blockage in the artery.
5. Physical Exertion and Extreme Activity
Intense physical exertion, particularly in individuals who are not accustomed to high levels of physical activity, has been linked to spontaneous coronary artery dissection. Heavy lifting, intense exercise, or extreme athletic activity can create sudden spikes in blood pressure, which may put stress on the coronary arteries. In some cases, this strain is enough to cause a tear in the arterial wall. It is essential for individuals with a predisposition to SCAD or arterial weaknesses to be cautious with physical activity.
6. Other Risk Factors
In addition to the above causes, several other factors may contribute to the development of coronary artery dissection:
Cigarette smoking: Smoking is a known risk factor for cardiovascular diseases and can weaken the arterial walls, making them more prone to dissection.
Chronic inflammation: Conditions like vasculitis (inflammation of the blood vessels) can damage the arteries and increase the risk of dissection.
Increased cholesterol levels: Elevated cholesterol can contribute to the development of atherosclerosis, which may increase the likelihood of an artery dissection.
High levels of stress: Emotional or physical stress has been shown to increase blood pressure, which can be a triggering factor for coronary artery dissection in susceptible individuals.
Symptoms of Coronary Artery Dissection
The symptoms of coronary artery dissection can vary depending on the severity of the dissection and the extent of blood flow restriction. Some common symptoms include:
Chest pain: Often described as a sharp or pressure-like pain, this is the most common symptom of a coronary artery dissection.
Shortness of breath: A decrease in blood flow to the heart muscle can result in difficulty breathing or shortness of breath.
Fatigue: Decreased oxygen supply to the heart can cause overwhelming fatigue or weakness.
Dizziness or fainting: If blood flow to the heart is significantly impaired, a person may feel dizzy or even faint.
In some cases, coronary artery dissection may be asymptomatic until it leads to a heart attack or other serious complications.
Treatment of Coronary Artery Dissection
The treatment for coronary artery dissection depends on the severity of the condition and the underlying cause. In many cases, conservative management is sufficient, including medications to manage blood pressure and prevent blood clots. In more severe cases, surgical interventions may be required.
Treatment options include:
Antiplatelet or anticoagulant therapy: To prevent clot formation.
Beta-blockers: To reduce the heart’s workload and blood pressure.
Coronary artery bypass grafting (CABG): In severe cases where the artery is blocked or severely damaged.
Conclusion
Coronary artery dissection is a rare but serious condition that can lead to severe cardiovascular complications. While the exact causes are still not fully understood, several factors contribute to the risk of developing this condition, including genetic predispositions, hormonal influences, and physical trauma.
Related topics: