Heart failure (HF) is a chronic and progressive condition where the heart’s ability to pump blood is weakened. As a result, the body’s organs and tissues may not receive adequate oxygen and nutrients, leading to a variety of symptoms, including fatigue, shortness of breath, and swelling in the legs and ankles. One of the lesser-discussed but significant consequences of heart failure is orthostatic hypotension (OH), a form of low blood pressure that occurs when standing up from a sitting or lying position.
This article will explore the relationship between heart failure and orthostatic hypotension, explaining how heart failure may contribute to this condition, the mechanisms behind it, and the clinical implications for patients. By understanding the link, healthcare providers can better manage heart failure patients and mitigate the risks associated with orthostatic hypotension.
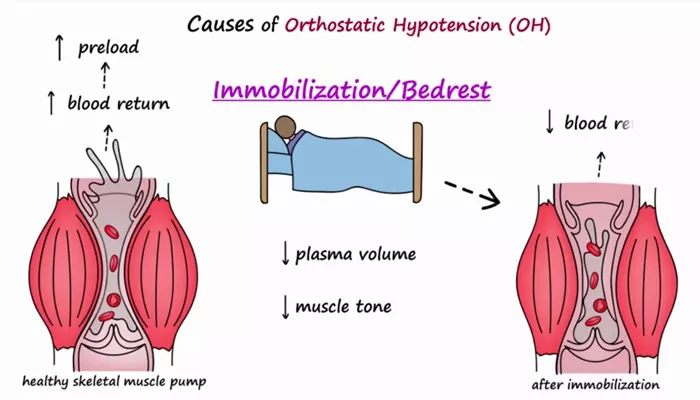
What Is Orthostatic Hypotension?
Orthostatic hypotension (OH) refers to a sudden drop in blood pressure when a person stands up after sitting or lying down.
Normally, when a person stands, gravity causes blood to pool in the lower extremities. The body compensates for this by constricting blood vessels and increasing heart rate to maintain blood flow to vital organs, especially the brain. In individuals with orthostatic hypotension, these compensatory mechanisms are either delayed or insufficient, resulting in dizziness, lightheadedness, and even fainting.
For diagnosis, orthostatic hypotension is defined as a decrease in systolic blood pressure of at least 20 mmHg or a decrease in diastolic blood pressure of at least 10 mmHg within three minutes of standing.
How Does Heart Failure Lead to Orthostatic Hypotension?
1. Impaired Circulatory Function
In heart failure, the heart is less effective at pumping blood. This results in reduced cardiac output, which can cause inadequate blood flow to the organs. The autonomic nervous system (ANS) plays a crucial role in regulating blood pressure.
In heart failure, this regulation is often disrupted, making it harder for the body to adjust blood pressure quickly when moving from a seated to a standing position.
Reduced cardiac output: The heart’s inability to pump blood efficiently means that there is less blood available to circulate through the body, especially when a person changes positions quickly.
Decreased blood flow to the brain: In heart failure, reduced blood flow can affect the brain’s ability to maintain normal function, which leads to dizziness and lightheadedness when standing.
2. Neurohormonal Activation
Heart failure activates several neurohormonal systems, including the sympathetic nervous system (SNS), the renin-angiotensin-aldosterone system (RAAS), and vasopressin. These systems are designed to help compensate for the heart’s reduced pumping ability by constricting blood vessels, increasing fluid retention, and stimulating the heart to beat faster.
However, the activation of these systems can also contribute to orthostatic hypotension in heart failure patients.
Increased vasodilation: Over time, chronic activation of these systems can lead to endothelial dysfunction, causing excessive vasodilation (relaxation of blood vessels). As a result, blood pressure may fall too low when a patient stands.
Impaired baroreceptor function: Baroreceptors are pressure-sensitive sensors in the blood vessels that help the body detect changes in blood pressure and make necessary adjustments. In heart failure, these receptors may become less responsive, reducing the ability to increase blood pressure when standing.
3. Medications Used in Heart Failure Treatment
Many of the medications prescribed to treat heart failure can also increase the risk of orthostatic hypotension. Some common heart failure medications that may contribute to this condition include:
Diuretics: Diuretics, or “water pills,” help reduce fluid buildup in the body by increasing urine production. While they are effective in treating fluid retention, they can also lead to dehydration, causing a drop in blood volume and blood pressure when standing.
Beta-blockers: These medications lower heart rate and reduce the workload on the heart. However, they can also impair the body’s ability to compensate for sudden drops in blood pressure, increasing the likelihood of orthostatic hypotension.
ACE inhibitors and Angiotensin II Receptor Blockers (ARBs): Both types of medication help to relax blood vessels and improve heart function.
However, they can also cause a sudden drop in blood pressure, particularly when standing up.
Vasodilators: Medications that relax blood vessels can help improve circulation but may cause a drop in blood pressure upon standing.
4. Fluid and Electrolyte Imbalances
Heart failure can lead to imbalances in fluids and electrolytes due to reduced kidney function or the use of diuretics. When the body does not have enough fluids, it can experience a drop in blood volume, which may contribute to orthostatic hypotension. Furthermore, electrolyte imbalances (such as low sodium or potassium) can impair the function of blood vessels and the heart, further exacerbating symptoms of low blood pressure.
Common Probabilities And Risk Factors for Orthostatic Hypotension in Heart Failure
Several factors can increase the likelihood of developing orthostatic hypotension in individuals with heart failure:
1. Severity of Heart Failure
The risk of orthostatic hypotension tends to be higher in individuals with advanced stages of heart failure, such as those with heart failure with reduced ejection fraction (HFrEF). In these patients, the heart’s pumping ability is significantly impaired, and they are more likely to experience a decrease in blood flow to the brain when standing.
Left ventricular dysfunction: The more severe the left ventricular dysfunction, the greater the likelihood of poor perfusion to vital organs, increasing the risk of orthostatic hypotension.
Right-sided heart failure: In right-sided heart failure, blood can back up into the systemic circulation, causing fluid retention and further compromising blood pressure regulation.
2. Age and Gender
Older adults with heart failure are particularly susceptible to orthostatic hypotension due to age-related changes in vascular tone and baroreceptor sensitivity. Additionally, elderly individuals often have comorbid conditions (such as diabetes or hypertension) that can exacerbate orthostatic hypotension.
Men with heart failure may also be at a higher risk compared to women, although this relationship is less clear.
3. Comorbidities
Individuals with comorbidities such as diabetes, renal dysfunction, or hypertension are at an increased risk of developing orthostatic hypotension. These conditions can worsen the circulatory and autonomic dysfunction associated with heart failure, further impairing the body’s ability to maintain normal blood pressure when standing.
Diabetes: Diabetic neuropathy can damage the autonomic nerves responsible for regulating blood pressure.
Chronic kidney disease: Kidney dysfunction often seen in heart failure can lead to fluid and electrolyte imbalances, which are risk factors for orthostatic hypotension.
4. The Use of Polypharmacy
Polypharmacy, or the use of multiple medications, is common in heart failure patients, especially those with other chronic conditions. The more medications a patient takes, the higher the risk of interactions that may lead to side effects, such as orthostatic hypotension.
Clinical Implications And Management
Managing orthostatic hypotension in heart failure patients requires a multidisciplinary approach. Below are some strategies to address this condition:
1. Adjusting Heart Failure Medications
Patients with heart failure may require adjustments to their medication regimen to reduce the risk of orthostatic hypotension. For example, reducing or carefully managing the use of diuretics can help minimize fluid loss. Adjusting beta-blocker doses or switching to other medications that have less impact on blood pressure regulation can also be beneficial.
2. Non-Pharmacological Interventions
Patients with heart failure and orthostatic hypotension can benefit from lifestyle changes such as:
Rising slowly: Encourage patients to rise slowly from a lying or sitting position to prevent sudden drops in blood pressure.
Compression stockings: These can help improve venous return and reduce blood pooling in the lower extremities.
Adequate hydration: Ensuring that patients stay hydrated can help maintain blood volume and prevent hypotension.
3. Monitoring and Regular Assessment
Heart failure patients should be closely monitored for signs of orthostatic hypotension, particularly during routine visits.
Blood pressure measurements in both sitting and standing positions can help identify any sudden drops in pressure.
Monitoring electrolyte levels is also essential to detect imbalances that may exacerbate hypotension.
Conclusion
In summary, heart failure can indeed cause orthostatic hypotension due to impaired circulatory function, neurohormonal dysregulation, medications, and fluid imbalances. Patients with advanced heart failure, older age, and additional comorbidities are particularly at risk. By understanding the mechanisms behind this condition, healthcare providers can better manage heart failure patients and reduce the risks associated with orthostatic hypotension.
Related topics: