Metformin is a commonly prescribed medication for managing type 2 diabetes mellitus (T2DM). It belongs to a class of drugs called biguanides and works by improving insulin sensitivity, reducing glucose production in the liver, and increasing glucose uptake in muscle tissues. While metformin is highly effective in managing blood glucose levels and is generally considered safe for most patients, it is contraindicated in patients with certain conditions, most notably heart failure (HF).
This article will explore the reasons behind this contraindication, providing an in-depth understanding of how metformin interacts with heart failure and the associated risks.
Understanding Metformin And Its Mechanism of Action
Metformin primarily functions by inhibiting hepatic glucose production, enhancing peripheral glucose uptake, and increasing insulin sensitivity.
It does not directly stimulate insulin secretion, which helps avoid the risk of hypoglycemia that can occur with other diabetic medications. Metformin’s mechanism of action is centered around activation of AMP-activated protein kinase (AMPK), which plays a key role in regulating energy metabolism in the liver and skeletal muscle.
Though metformin is effective at controlling blood sugar, it is not without risks. One of the most critical concerns is its contraindication in certain cardiovascular conditions, particularly heart failure.
The Pathophysiology of Heart Failure
Heart failure is a complex condition characterized by the heart’s inability to pump blood efficiently to meet the body’s metabolic demands. It can result from a variety of underlying causes, including coronary artery disease, hypertension, valvular heart disease, and myocardial infarction. Patients with heart failure often experience symptoms such as shortness of breath, fatigue, fluid retention, and reduced exercise tolerance.
The pathophysiology of heart failure involves a combination of factors, including:
Decreased Cardiac Output: Due to impaired heart muscle function, the heart is unable to pump sufficient blood, leading to decreased tissue perfusion.
Increased Sympathetic Activity: The body attempts to compensate by increasing heart rate and vasoconstriction, which can exacerbate the problem.
Fluid Retention: Inadequate kidney perfusion activates the renin-angiotensin-aldosterone system, leading to sodium and water retention, contributing to edema and worsening symptoms.
Altered Oxygen Delivery: The heart’s reduced ability to circulate blood leads to diminished oxygen delivery to tissues, increasing the risk of ischemia and exacerbating fatigue.
Given the complex interplay of factors involved in heart failure, certain medications can have unintended consequences that worsen the condition. Metformin, while effective for managing diabetes, is one such drug that can be particularly harmful in patients with heart failure.
Why Is Metformin Contraindicated in Heart Failure?
Metformin is contraindicated in heart failure primarily due to the risk of lactic acidosis, a potentially fatal condition that occurs when there is an accumulation of lactate in the blood. In patients with heart failure, the following mechanisms can increase the risk of lactic acidosis when metformin is used:
1. Impaired Renal Function
The kidneys play a crucial role in excreting metformin from the body. In patients with heart failure, renal function is often compromised due to decreased perfusion and poor blood flow. This can lead to metformin accumulation in the bloodstream, as the drug is not cleared efficiently.
When metformin levels become too high, it can impair mitochondrial function in cells, leading to the accumulation of lactate.
In normal circumstances, lactate is produced by muscles and red blood cells during anaerobic metabolism. It is usually converted to glucose by the liver or cleared through the kidneys. However, in patients with heart failure and compromised renal function, the liver’s ability to clear lactate is reduced, and the kidneys cannot efficiently excrete it, leading to lactic acidosis.
2. Hypoxia and Tissue Perfusion
Heart failure often results in diminished oxygen supply to tissues (hypoxia), which can exacerbate the metabolic changes associated with lactic acid production. In such a state, cells rely more heavily on anaerobic metabolism for energy, leading to increased lactate production. When metformin is used in this context, the drug may further impair the body’s ability to clear lactate, increasing the risk of acidosis.
The kidneys, already under stress due to the heart’s inability to maintain adequate perfusion, may not function optimally to eliminate lactate from the blood. This creates a dangerous environment for the development of lactic acidosis, a rare but serious side effect of metformin therapy.
3. Decreased Hepatic Function
In advanced stages of heart failure, liver function can be compromised as blood flow to the liver diminishes. The liver is vital for processing and detoxifying substances, including lactate. If the liver cannot adequately clear lactate from the bloodstream, it can accumulate, resulting in metabolic acidosis. The combination of impaired liver function and compromised renal clearance significantly raises the risk of developing lactic acidosis in patients taking metformin.
4. Dehydration and Electrolyte Imbalance
Heart failure is often associated with fluid imbalances, including dehydration due to diuretic use or fluid loss from the body’s inability to circulate blood effectively. Dehydration can impair renal function, which further reduces the clearance of metformin. The resulting electrolyte imbalances, including low sodium, potassium, and chloride levels, can also contribute to the development of metabolic acidosis. Metformin’s side effect profile in such patients can be exacerbated under these conditions, increasing the risk of lactic acidosis.
5. Increased Risk in Severe Heart Failure
In patients with severe heart failure (particularly those with a low ejection fraction), the risk of metformin-associated lactic acidosis becomes even more significant. In these patients, the body’s ability to compensate for low cardiac output and impaired oxygen delivery is severely limited. The combination of reduced perfusion to the kidneys, liver, and other vital organs makes the body less capable of processing and eliminating metformin, leading to a dangerous buildup of the drug and an increased risk of lactic acidosis.
Symptoms of Lactic Acidosis
Lactic acidosis is a medical emergency that requires immediate intervention. Symptoms can include:
- Severe nausea and vomiting
- Abdominal pain
- Rapid breathing (tachypnea)
- Weakness and fatigue
- Muscle pain
- Confusion or altered mental status
- Low blood pressure and shock
If left untreated, lactic acidosis can progress to organ failure, coma, and death. For this reason, metformin is contraindicated in patients with heart failure, especially those with impaired renal function or advanced stages of the disease.
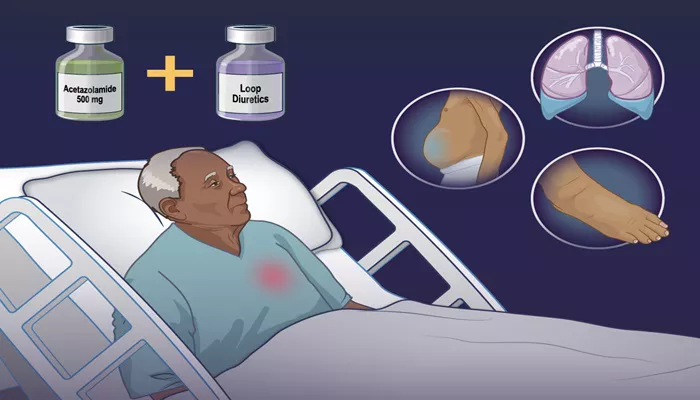
Alternatives to Metformin for Patients with Heart Failure
For patients with heart failure and type 2 diabetes, there are alternative medications that may be safer and more effective.
These include:
1. SGLT2 Inhibitors
Sodium-glucose co-transporter 2 (SGLT2) inhibitors, such as empagliflozin and dapagliflozin, are a newer class of drugs that have been shown to improve both glycemic control and cardiovascular outcomes in patients with heart failure. SGLT2 inhibitors work by preventing glucose reabsorption in the kidneys, leading to glucose excretion in the urine. They have also been shown to reduce the risk of hospitalization for heart failure and improve kidney function in patients with diabetes and heart failure.
2. GLP-1 Receptor Agonists
Glucagon-like peptide-1 (GLP-1) receptor agonists, such as liraglutide and semaglutide, are another class of medications that have been shown to reduce blood sugar levels and provide cardiovascular benefits in patients with type 2 diabetes.
These medications enhance insulin secretion and improve glucose metabolism while also promoting weight loss and reducing blood pressure.
3. Insulin Therapy
In cases where oral medications are not sufficient, insulin therapy may be used to control blood glucose levels. While insulin does not have the same cardiovascular benefits as some newer agents, it remains an effective treatment for managing diabetes in patients with heart failure, provided it is used cautiously and monitored closely.
Conclusion
Metformin is a cornerstone in the treatment of type 2 diabetes, but its use in patients with heart failure is contraindicated due to the increased risk of lactic acidosis. This life-threatening condition can occur due to impaired renal and hepatic function, poor tissue perfusion, and the physiological changes associated with heart failure. Understanding the pathophysiological mechanisms behind this contraindication is crucial for healthcare providers to ensure safe and effective diabetes management in patients with heart failure.
Related topics: