Supraventricular Tachycardia (SVT) is a type of abnormal heart rhythm or arrhythmia. It occurs when there is a malfunction in the electrical pathways of the heart, causing it to beat faster than normal. In most cases, the heart rate can exceed 100 beats per minute, and it can even reach rates of 200 beats per minute or more. SVT can happen suddenly and can be brief or last for an extended period. This article will explore how SVT happens, including the causes, risk factors, symptoms, and possible treatments.
The Heart’s Electrical System: A Brief Overview
To understand how SVT occurs, it’s important to first understand how the heart beats. The heart’s electrical system controls the timing and rhythm of each heartbeat. It consists of specialized cells that generate electrical impulses, which help the heart contract and pump blood effectively.
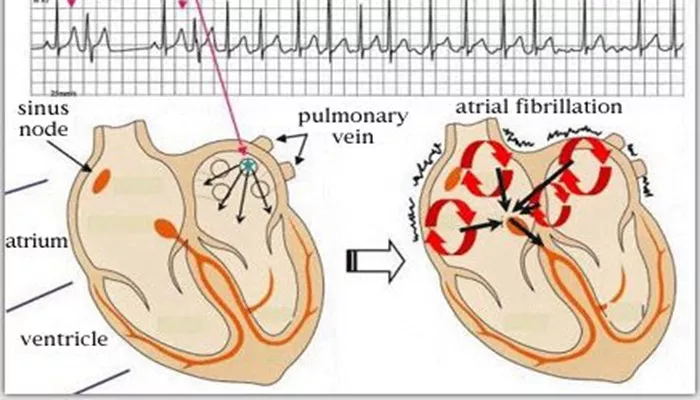
The process begins in the sinoatrial (SA) node, a group of cells located in the right atrium of the heart. The SA node acts as the heart’s natural pacemaker, generating electrical signals that travel through the heart’s conduction system, causing the heart muscles to contract. These electrical signals first move through the atria, causing them to contract and push blood into the ventricles. The signal then travels to the atrioventricular (AV) node, which temporarily slows it down before sending it to the ventricles, allowing them to contract and pump blood to the rest of the body.
In SVT, there is an issue with this electrical conduction system. The heart’s normal rhythm is disrupted, causing the heart to beat too quickly and often too erratically.
How Does SVT Happen?
SVT occurs when there is a problem with the electrical pathways in the heart that causes the heart to beat at an unusually fast rate. This happens because of an abnormal electrical circuit or an extra pathway in the heart. These disruptions can be triggered in a few different ways.
1. Abnormal Electrical Circuits (Re-entry Arrhythmias)
One of the most common causes of SVT is a phenomenon called re-entry arrhythmia. This occurs when the electrical signal in the heart loops back on itself instead of following its normal path. When the signal is blocked in one area, it can travel in the opposite direction, causing the heart to contract repeatedly and at a faster rate. This creates a cycle of abnormal electrical impulses.
In the case of SVT, the abnormal circuit often involves the atria (the upper chambers of the heart) and the AV node (which acts as the relay station between the atria and ventricles). This creates a situation where the heart may beat in an uncoordinated manner, leading to rapid heart rates.
2. Extra Pathways (Accessory Pathways)
Another common cause of SVT involves extra electrical pathways in the heart. These extra pathways can form between the atria and ventricles, bypassing the normal conduction system. When these extra pathways are present, they can lead to electrical signals traveling abnormally between the atria and ventricles. This causes the heart to beat very quickly.
An example of this condition is Wolff-Parkinson-White syndrome (WPW). This is a congenital condition in which an extra electrical pathway exists, allowing for an abnormal electrical circuit that can result in episodes of SVT. The presence of these extra pathways makes the heart more prone to fast rhythms.
3. Abnormalities in the AV Node (AV Nodal Reentrant Tachycardia)
Another mechanism behind SVT is AV nodal reentrant tachycardia (AVNRT). In this condition, the AV node, which normally regulates electrical signals between the atria and ventricles, develops two pathways. One pathway is fast, and the other is slow. If the electrical signal travels down the slow pathway and then loops back around to the fast pathway, a re-entry circuit is created, leading to a rapid heartbeat.
AVNRT is one of the most common causes of SVT, especially in adults. It is often triggered by stress, alcohol, or caffeine consumption.
4. Increased Automaticity
In some cases of SVT, the rapid heart rate is caused by increased automaticity in certain areas of the heart. Normally, the SA node is the only area of the heart that generates electrical impulses, but in certain circumstances, other cells in the heart can begin to generate electrical signals independently, leading to an abnormal increase in heart rate. This is less common in SVT but can occur in some cases.
5. Triggered Activity
In addition to the mechanisms mentioned above, triggered activity is another factor that can lead to SVT. Triggered activity occurs when a heart cell generates an electrical impulse at the wrong time, often after the normal contraction. These impulses can propagate through the heart, causing it to beat too quickly. This type of SVT can sometimes be seen in people with certain heart conditions, electrolyte imbalances, or after certain medications.
Risk Factors for SVT
Several factors can increase the risk of developing SVT. These include:
Age: SVT can occur at any age, but it is more common in young adults.
Heart conditions: People with heart disease or structural abnormalities in the heart may be at higher risk.
Congenital conditions: Some individuals are born with abnormalities in the heart’s electrical system, such as WPW syndrome, which increases the likelihood of SVT.
Stimulants: Caffeine, alcohol, and certain drugs (such as cocaine) can trigger episodes of SVT.
Stress and anxiety: Emotional or physical stress can contribute to the onset of SVT.
Family history: A family history of arrhythmias can increase the risk of SVT.
Symptoms of SVT
SVT can develop suddenly and often without warning. The symptoms vary from person to person, but common signs of SVT include:
Palpitations: A sensation of a fast or irregular heartbeat.
Dizziness or lightheadedness: Due to the heart’s inability to pump blood effectively during rapid beats.
Shortness of breath: Difficulty breathing during an episode of SVT.
Chest pain or tightness: This can occur in some cases, especially if the SVT episode is prolonged or if there is an underlying heart condition.
Fatigue: Feeling unusually tired or weak during or after an episode.
While most episodes of SVT are not life-threatening, they can cause discomfort and concern. In rare cases, if the episode is prolonged or the individual has other heart conditions, SVT can lead to more serious complications.
Treatment for SVT
Treatment for SVT varies depending on the underlying cause and the severity of the condition. Common treatment options include:
Vagal maneuvers: Techniques like coughing, bearing down (as if having a bowel movement), or splashing cold water on the face can sometimes help slow down the heart rate by stimulating the vagus nerve.
Medications: Beta-blockers or calcium channel blockers may be used to control the heart rate during an episode.
Adenosine: This medication can be given intravenously to reset the heart’s electrical system during an SVT episode.
Cardioversion: In some cases, if the episode does not resolve with medications, electrical cardioversion may be used to restore a normal rhythm.
Catheter ablation: This is a more permanent solution for people who experience frequent episodes of SVT. It involves using a catheter to destroy the abnormal electrical pathways causing the arrhythmia.
Conclusion
Supraventricular Tachycardia (SVT) is a condition in which the heart beats faster than normal due to abnormal electrical activity. The mechanisms behind SVT are primarily related to issues in the heart’s electrical pathways, including re-entry arrhythmias, extra pathways, and abnormal electrical activity. While SVT is generally not life-threatening, it can cause significant discomfort and may require treatment in some cases. With appropriate management, most individuals with SVT can lead a normal, active life.
Related topics: