Myocarditis is an inflammatory condition of the heart muscle (myocardium) that can lead to significant damage if not diagnosed and treated properly. It is often caused by infections, most commonly viral infections, but it can also result from autoimmune diseases, toxins, or even certain medications. The inflammation in myocarditis can impair the heart’s ability to pump blood effectively, which may lead to heart failure or arrhythmias in severe cases.
One of the most common biomarkers used to evaluate inflammation in the body is C-reactive protein (CRP). CRP is produced by the liver in response to inflammatory signals, particularly those initiated by cytokines such as interleukin-6 (IL-6). Because CRP levels rise significantly in response to inflammation, it is commonly used as an indicator of acute inflammation or infection. This raises an important question: Is CRP elevated in myocarditis? In this article, we will explore how CRP levels behave in myocarditis, the potential causes behind these changes, and how CRP can aid in the diagnosis and management of this serious condition.
What Is CRP?
C-reactive protein (CRP) is a protein that circulates in the blood and is produced by the liver in response to inflammation. It belongs to a group of proteins called acute-phase reactants, which are substances that increase or decrease in the blood during inflammation or infection.
CRP levels are typically measured through a simple blood test. Under normal circumstances, CRP levels are low in the blood, generally below 1 mg/L. However, during inflammation or infection, CRP levels can rise dramatically, sometimes reaching hundreds of milligrams per liter. This increase makes CRP a useful biomarker in detecting conditions that cause systemic inflammation.
What Is Myocarditis?
Myocarditis refers to inflammation of the heart muscle, which can interfere with the heart’s ability to pump blood. The condition can range from mild to severe, with symptoms including chest pain, fatigue, shortness of breath, and heart palpitations. If left untreated, myocarditis can lead to more serious complications, such as heart failure, arrhythmias, or even sudden cardiac death.
Infections, particularly viral infections, are the most common cause of myocarditis. Other potential causes include bacterial infections, autoimmune diseases (such as lupus), exposure to toxins, and certain medications. Regardless of the cause, the underlying issue in myocarditis is always inflammation of the myocardium.
CRP in Inflammatory Conditions
CRP is a nonspecific marker of inflammation, which means that elevated CRP levels can indicate the presence of many different inflammatory conditions. For example, CRP levels rise in response to bacterial infections, autoimmune diseases like rheumatoid arthritis, and even in cases of trauma or surgery. It is important to note that while CRP is elevated in inflammation, it does not tell us the specific cause of that inflammation.
Because myocarditis is an inflammatory condition, CRP levels are typically elevated in individuals with this diagnosis.
However, the degree to which CRP levels rise can vary depending on the severity of the myocarditis and the underlying cause.
Is CRP Elevated in Myocarditis?
Yes, CRP is often elevated in myocarditis, but the degree of elevation can vary depending on several factors. Studies have shown that CRP levels are often elevated in patients with myocarditis, especially during the acute phase of the disease. In some cases, CRP levels may be significantly higher in patients with severe myocarditis, while in others with mild cases, CRP levels may only show a moderate increase.
Why Is CRP Elevated in Myocarditis?
CRP levels rise in response to inflammatory cytokines such as interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha). These cytokines are released during inflammation, and they stimulate the liver to produce CRP. In the case of myocarditis, the inflammation in the myocardium triggers the release of these cytokines into the bloodstream, leading to the elevated CRP levels.
Role of CRP in the Diagnosis of Myocarditis
While CRP is a helpful marker of inflammation, it is important to remember that it is not specific to myocarditis. Elevated CRP levels can occur in a variety of conditions, including other forms of heart disease, infections, and autoimmune disorders. As such, CRP alone cannot be used to definitively diagnose myocarditis.
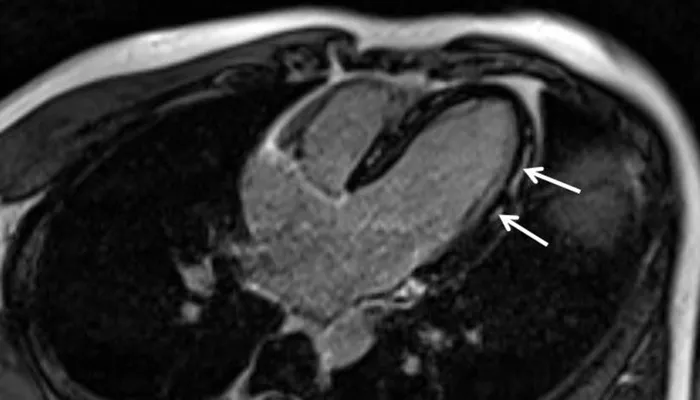
However, CRP can be a useful adjunct to other diagnostic tools. When combined with clinical symptoms (such as chest pain, fatigue, and shortness of breath), imaging studies (such as echocardiograms or MRIs), and other laboratory tests (like troponin levels), CRP can help physicians assess the degree of inflammation and make a more accurate diagnosis of myocarditis.
CRP vs. Other Biomarkers in Myocarditis
In addition to CRP, other biomarkers may be elevated in myocarditis. The most important of these is troponin, a protein released from heart muscle cells when they are damaged. Elevated troponin levels are indicative of heart muscle injury, and they are often used to assess the severity of myocarditis. Unlike CRP, which indicates general inflammation, troponin levels are more specific to heart muscle damage and can help differentiate myocarditis from other causes of chest pain, such as a heart attack.
Procalcitonin is another biomarker that may be elevated in cases of infection, particularly bacterial infections. However, it is less commonly used in the diagnosis of myocarditis, as viral infections are more common causes of the condition.
CRP And The Prognosis of Myocarditis
In patients with myocarditis, CRP levels may be associated with prognosis. Studies have shown that higher CRP levels at the time of diagnosis may correlate with a more severe disease course and worse outcomes. Elevated CRP levels have been linked to an increased risk of heart failure, arrhythmias, and even death in patients with myocarditis.
Because CRP levels reflect the extent of systemic inflammation, higher levels may indicate more widespread inflammation that could lead to greater damage to the heart muscle. As such, CRP can provide valuable information about the severity of the condition and can help doctors determine the best course of treatment.
CRP in Monitoring Disease Progression
CRP can also be useful in monitoring the progression of myocarditis. After treatment, CRP levels are often tracked to assess how well the inflammation is responding to therapy. A decrease in CRP levels over time may indicate that the inflammation is subsiding and that the treatment is effective. Conversely, persistently high CRP levels or a rebound increase in CRP levels may suggest that the myocarditis is not improving, or that complications are developing.
Limitations of CRP in Myocarditis
While CRP is a valuable tool for detecting inflammation, it has its limitations. As mentioned earlier, CRP is a nonspecific marker, meaning that it cannot definitively indicate the presence of myocarditis or any other specific condition. Elevated CRP levels can also occur in conditions such as:
- Infections (bacterial, viral, fungal, etc.)
- Autoimmune diseases (rheumatoid arthritis, lupus)
- Trauma or surgery
- Cancer
Therefore, CRP levels must always be interpreted in conjunction with clinical findings and other diagnostic tests. Relying solely on CRP for diagnosis could lead to misdiagnosis or delayed treatment.
Treatment of Myocarditis and CRP
Treatment of myocarditis depends on the underlying cause and the severity of the disease. In most cases, treatment involves supportive care to help the heart recover, along with medications to control inflammation. If a viral infection is the cause, antiviral medications may be prescribed. If an autoimmune disease is responsible, immunosuppressive medications may be necessary.
The role of CRP in the treatment process is largely as a monitoring tool. By tracking CRP levels during treatment, physicians can determine how well the body is responding to therapy and adjust the treatment plan as needed.
Conclusion
In summary, CRP is elevated in myocarditis, as it is in many inflammatory conditions. However, because CRP is a nonspecific marker of inflammation, it cannot be used alone to diagnose myocarditis. When combined with other diagnostic tools and clinical symptoms, elevated CRP levels can help physicians assess the degree of inflammation and guide treatment decisions. CRP can also provide valuable information about the prognosis and progression of the disease, helping doctors monitor the effectiveness of therapy and detect potential complications.
Though CRP is useful in the context of myocarditis, it is not without its limitations. Elevated CRP levels alone cannot confirm the presence of myocarditis or determine its cause, and further testing is always required to arrive at a definitive diagnosis. Nevertheless, CRP remains an important biomarker in the evaluation of myocarditis and other inflammatory conditions, playing a key role in the clinical management of these diseases.
Related topics: