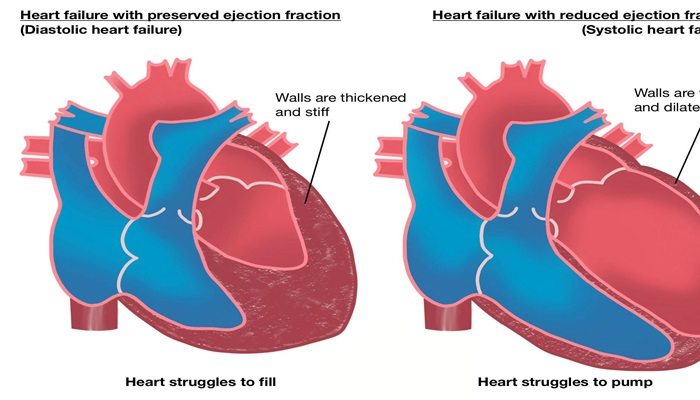
Diastolic heart failure, also known as heart failure with preserved ejection fraction (HFpEF), is a significant cardiovascular condition characterized by the heart’s inability to relax adequately during the diastolic phase of the cardiac cycle. This condition leads to insufficient filling of the left ventricle, resulting in reduced blood flow to the body despite a normal ejection fraction. As a cardiologist, it is crucial to understand the indicators, symptoms, diagnostic criteria, and management strategies associated with diastolic heart failure.
What Is Diastolic Heart Failure?
Diastolic heart failure occurs when the left ventricle becomes stiff and cannot relax properly. This stiffness prevents the heart from filling with blood efficiently during the diastole phase, which is when the heart muscle relaxes and allows chambers to fill with blood. Consequently, less blood is pumped out to the body during systole (the contraction phase), leading to various symptoms and complications.
Symptoms of Diastolic Heart Failure
The symptoms of diastolic heart failure can often mimic those of systolic heart failure. Common signs include:
Shortness of Breath: Patients often experience difficulty breathing during physical exertion or when lying flat (orthopnea) due to fluid accumulation in the lungs.
Fatigue and Weakness: Reduced blood flow can lead to feelings of tiredness and decreased exercise tolerance.
Swelling: Patients may notice swelling in their legs, ankles, or abdomen due to fluid retention.
Coughing or Wheezing: A persistent cough, especially when lying down, can occur due to pulmonary congestion.
Rapid Heartbeat: An irregular heartbeat may be present as the heart attempts to compensate for reduced efficiency.
Causes And Risk Factors
Several factors contribute to the development of diastolic heart failure:
Aging: As individuals age, their heart and blood vessels become less elastic, increasing the risk of stiffness in the heart muscle.
Hypertension: Chronic high blood pressure forces the heart to work harder, leading to thickening and stiffening of the ventricular walls.
Diabetes: This condition can cause changes in the heart muscle that contribute to stiffness.
Coronary Artery Disease: Reduced blood flow to the heart muscle can lead to its dysfunction.
Obesity and Sedentary Lifestyle: Excess weight and lack of physical activity increase cardiovascular strain.
Diagnosis of Diastolic Heart Failure
Diagnosing diastolic heart failure involves a combination of clinical evaluation and diagnostic tests. The following steps are typically undertaken:
Medical History and Physical Examination: A thorough assessment of symptoms, medical history, and physical examination findings such as jugular venous distension or peripheral edema.
Echocardiogram: This imaging test is essential for assessing left ventricular function. It helps determine ejection fraction and can reveal signs of diastolic dysfunction such as abnormal relaxation patterns or increased left atrial size.
Blood Tests: These tests can help rule out other causes of symptoms and assess kidney function and electrolyte levels.
Electrocardiogram (EKG): An EKG can identify arrhythmias or other electrical issues within the heart.
Chest X-ray: This imaging can show signs of fluid buildup in the lungs or other structural abnormalities.
To confirm a diagnosis of diastolic heart failure, three criteria must be met:
Presence of signs or symptoms consistent with heart failure (e.g., dyspnea, fatigue).
Normal or mildly reduced left ventricular ejection fraction (typically >50%).
Evidence of impaired left ventricular relaxation or elevated filling pressures.
Management Strategies
While there is no cure for diastolic heart failure, effective management strategies can improve symptoms and enhance quality of life:
Lifestyle Modifications
Dietary Changes: Adopting a heart-healthy diet low in sodium can help manage blood pressure and reduce fluid retention.
Regular Exercise: Engaging in regular physical activity tailored to individual capability can improve overall cardiovascular health.
Weight Management: Achieving and maintaining a healthy weight
reduces strain on the heart.
Smoking Cessation: Quitting smoking significantly lowers cardiovascular risk.
Pharmacological Treatments
Medications play a crucial role in managing symptoms associated with diastolic heart failure:
Diuretics: These medications help reduce fluid retention by promoting urine production.
Antihypertensive Agents: Medications such as ACE inhibitors or angiotensin receptor blockers (ARBs) are used to control high blood pressure.
SGLT2 Inhibitors: Originally developed for diabetes management, these drugs have shown promise in improving outcomes for patients with HFpEF by enhancing cardiac efficiency.
Monitoring and Follow-Up
Regular follow-up appointments are essential for monitoring symptom progression, medication effectiveness, and adjusting treatment plans as needed. Patients should be educated about recognizing worsening symptoms that may require immediate medical attention.
Conclusion
Diastolic heart failure represents a significant health concern that requires careful diagnosis and management. By understanding its symptoms, causes, diagnostic criteria, and treatment options, healthcare providers can better support patients living with this condition. Ongoing research into effective therapies continues to evolve our understanding and management strategies for diastolic heart failure, offering hope for improved outcomes for affected individuals.
In summary, recognizing the signs indicative of diastolic heart failure is vital for timely intervention. By addressing risk factors through lifestyle modifications and pharmacological treatments, patients can achieve better control over their condition and enhance their quality of life.
Related topics: