Hypertension, or high blood pressure, is one of the most prevalent chronic conditions in adults globally. It is a significant risk factor for various cardiovascular diseases, including heart attacks, strokes, and heart failure. As hypertension can often be asymptomatic, it’s often referred to as the “silent killer.” Nursing care plays a crucial role in managing patients with hypertension, aiming to reduce blood pressure levels and mitigate long-term complications. A comprehensive nursing care plan for hypertension focuses on education, medication adherence, lifestyle modifications, and monitoring, ensuring holistic management for the patient.
This article will outline a professional nursing care plan for a patient with hypertension, providing insight into the essential components, interventions, and considerations that contribute to effective management.
Understanding Hypertension and Its Impact
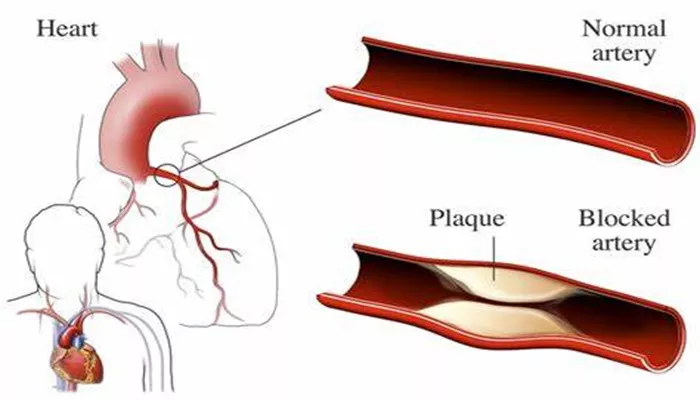
Hypertension is defined as having a consistent reading of systolic blood pressure (SBP) of 130 mmHg or higher, or diastolic blood pressure (DBP) of 80 mmHg or higher. Over time, sustained high blood pressure can damage blood vessels, increasing the risk of heart disease, kidney damage, and vision problems. Hypertension is typically classified into two types:
Primary (Essential) Hypertension: This form of hypertension has no identifiable cause and is the most common.
Secondary Hypertension: Caused by an underlying condition, such as kidney disease, hormonal disorders, or medications.
Nurses play a key role in identifying hypertension early, managing ongoing care, and educating patients on effective ways to control their condition.
Nursing Assessment for Hypertension
The first step in developing an appropriate nursing care plan is performing a thorough patient assessment. This involves evaluating both subjective and objective data.
Subjective Data
Health history: The nurse gathers a detailed health history to understand any contributing factors such as family history of hypertension, previous diagnoses, or underlying health conditions (e.g., diabetes, kidney disease).
Patient’s lifestyle: Information on diet, exercise habits, alcohol consumption, and smoking provides insights into modifiable risk factors for hypertension.
Symptoms: While hypertension often has no symptoms, some patients may report headaches, dizziness, or shortness of breath.
Objective Data
Blood pressure measurement: Regular monitoring of blood pressure is critical. Accurate readings must be taken at least twice on separate occasions to confirm a diagnosis of hypertension.
Physical examination: A full examination helps identify signs of organ damage, including heart murmur, eye changes, or signs of kidney involvement.
Laboratory tests: Blood tests and urine analysis may be ordered to assess kidney function, cholesterol levels, and electrolyte balance.
Nursing Diagnosis for Hypertension
Based on the assessment, the nurse formulates nursing diagnoses that guide the care plan. Common nursing diagnoses for a patient with hypertension include:
Ineffective Health Management: Due to a lack of knowledge or motivation to adhere to a treatment regimen.
Risk for Decreased Cardiac Output: Related to hypertension, which increases the workload on the heart.
Anxiety: Patients may experience anxiety due to their diagnosis, possible complications, or lifestyle changes.
Risk for Impaired Kidney Function: Related to prolonged hypertension, which may cause kidney damage.
Nursing Interventions for Hypertension
Once the nursing diagnoses are identified, the nurse will implement various interventions to address the patient’s needs.
1. Blood Pressure Monitoring and Management
Frequent monitoring: Nurses will ensure that blood pressure is monitored regularly to track changes and evaluate the effectiveness of prescribed interventions.
Medication management: Administer antihypertensive medications as prescribed (e.g., diuretics, ACE inhibitors, beta-blockers). Educate patients about the importance of medication adherence and possible side effects.
Teach proper technique: Instruct patients on how to measure their own blood pressure at home, emphasizing correct cuff size, posture, and time of measurement.
2. Educating Patients on Lifestyle Modifications
Dietary changes: Educate patients on adopting a low-sodium, heart-healthy diet such as the DASH (Dietary Approaches to Stop Hypertension) diet. Encourage reducing intake of processed foods, alcohol, and caffeine.
Exercise: Encourage patients to engage in moderate-intensity aerobic exercises such as walking or swimming for at least 30 minutes on most days of the week. Exercise helps lower blood pressure and improve cardiovascular health.
Weight management: Help patients set realistic goals for weight loss, as even a small reduction in weight can significantly lower blood pressure.
Smoking cessation: Smoking is a major risk factor for hypertension and cardiovascular diseases. Offer resources and support for quitting smoking.
3. Promoting Medication Adherence
Address barriers: Identify factors that may impede medication adherence, such as cost, forgetfulness, or side effects. Offer solutions such as pillboxes, reminder systems, or community resources.
Reinforce the importance: Continuously remind patients that medications are vital for managing hypertension and preventing complications like stroke or kidney failure.
4. Monitoring for Complications
Assess for symptoms of organ damage: Nurses should assess for signs of heart failure (e.g., shortness of breath, edema), kidney impairment (e.g., changes in urine output, swelling), and stroke (e.g., sudden weakness or confusion).
Regular screenings: Advise patients to undergo regular screenings for cholesterol, blood sugar, and kidney function tests.
5. Psychological Support and Stress Management
Coping strategies: Hypertension often leads to anxiety due to the fear of complications. Nurses can offer stress-reduction techniques such as deep breathing, meditation, and progressive muscle relaxation.
Provide reassurance: Provide emotional support to help patients understand that hypertension can be managed effectively with proper care.
Nursing Goals for Hypertension
Nursing goals are essential in providing clear direction for patient care.
For a patient with hypertension, the following goals may be established:
Reduce blood pressure: Achieve and maintain a target blood pressure of less than 130/80 mmHg.
Enhance patient knowledge: Ensure the patient understands hypertension, its complications, and the importance of treatment and lifestyle modifications.
Promote adherence to the treatment plan: The patient should demonstrate consistent medication adherence, dietary changes, and participation in physical activity.
Prevent complications: Minimize the risk of complications such as stroke, kidney damage, and heart failure.
Evaluating the Effectiveness of the Nursing Care Plan
To evaluate the success of the nursing care plan, nurses will assess the patient’s progress toward achieving the set goals.
This evaluation may include:
Blood pressure readings: Monitor if the patient’s blood pressure has decreased to within the target range.
Patient understanding: Assess whether the patient has gained sufficient knowledge about hypertension management and can explain the importance of lifestyle changes and medication.
Behavioral changes: Evaluate the patient’s ability to adopt recommended lifestyle modifications such as improved diet, increased physical activity, and smoking cessation.
Complications: Monitor the patient for any signs of organ damage or other complications related to hypertension.
Conclusion
Hypertension is a prevalent and serious health condition that requires ongoing management and vigilance. The nursing care plan for a patient with hypertension involves a multi-faceted approach, focusing on blood pressure management, lifestyle modifications, medication adherence, and psychological support. Nurses must provide comprehensive education, monitor for complications, and collaborate with the healthcare team to optimize patient outcomes.
Related topics: