Pericarditis and Myocardial Infarction (MI) are both serious heart conditions, but they are fundamentally different.
Understanding the distinction between the two is crucial for accurate diagnosis and appropriate treatment. Both conditions present with chest pain, but the characteristics of this pain, along with other key clinical signs, can help clinicians differentiate between them.
In this article, we will explore the differences between Pericarditis and MI, focusing on their clinical features, diagnostic methods, and treatment options. It is important for healthcare providers to be able to distinguish between the two to ensure the best possible outcomes for patients.
What Is Pericarditis?
Pericarditis is inflammation of the pericardium, the double-layered sac that surrounds the heart. The condition can be acute or chronic and may be caused by viral infections, bacterial infections, autoimmune diseases, or even trauma. The inflammation can lead to chest pain, fever, and other symptoms. Pericarditis can be categorized into various types based on the underlying cause, including viral, bacterial, and idiopathic pericarditis.
The main symptom of pericarditis is sharp, stabbing chest pain. This pain often gets worse when a person is lying down or breathing deeply, and it is relieved by sitting up or leaning forward. Other symptoms may include shortness of breath, a dry cough, and a feeling of weakness or fatigue.
What Is Myocardial Infarction (MI)?
Myocardial Infarction, commonly known as a heart attack, occurs when blood flow to a part of the heart muscle is blocked, usually by a blood clot. This leads to a lack of oxygen in the affected heart muscle, causing damage or death of the tissue. MI is primarily caused by coronary artery disease, where fatty deposits (plaques) clog the arteries that supply blood to the heart.
The hallmark symptom of MI is chest pain, but it is typically described as a pressure or squeezing sensation rather than the sharp, stabbing pain seen in pericarditis. The pain often radiates to other parts of the body, such as the left arm, neck, or jaw, and it is associated with other symptoms like nausea, sweating, dizziness, and shortness of breath.
Key Differences in Symptoms
While both conditions can cause chest pain, there are key differences in the nature of the pain:
Pericarditis Pain: The pain is often sharp and pleuritic (worse with breathing and coughing). It may also worsen when the person is lying flat and is relieved by sitting up or leaning forward.
MI Pain: The pain is typically described as a pressure or tightness in the chest. It may be more intense and constant and is often accompanied by a feeling of impending doom. The pain can radiate to other areas such as the left arm, back, neck, or jaw.
Diagnostic Techniques to Differentiate Pericarditis And MI
Both pericarditis and MI are serious conditions, but they require different diagnostic approaches. A healthcare provider will typically start with a thorough medical history, physical examination, and various tests to help differentiate the two.
1. Electrocardiogram (ECG or EKG)
An electrocardiogram (ECG) is one of the most important tools used to assess heart conditions. Both pericarditis and MI can show changes on an ECG, but the patterns are distinct:
Pericarditis ECG Findings: The ECG in pericarditis often shows diffuse ST-segment elevation across many leads, as well as PR-segment depression. This is characteristic of the inflammation of the pericardium. The changes may be widespread and not localized to a specific area of the heart.
MI ECG Findings: In contrast, MI typically shows localized ST-segment elevation or depression depending on the part of the heart affected. If the patient is having an acute MI, there will often be abnormal Q waves, and the ST-segment elevation will be confined to specific leads that correspond to the region of the heart involved.
2. Blood Tests
Pericarditis Blood Tests: Blood tests in pericarditis may show mild elevations in inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). However, cardiac enzymes (troponin and CK-MB) are usually normal or only mildly elevated in pericarditis.
MI Blood Tests: In contrast, myocardial infarction leads to a significant rise in cardiac enzymes, particularly troponin.
Troponin is a protein released when the heart muscle is damaged. Elevated levels of troponin, especially when sustained, are a strong indication of an MI.
3. Imaging Tests
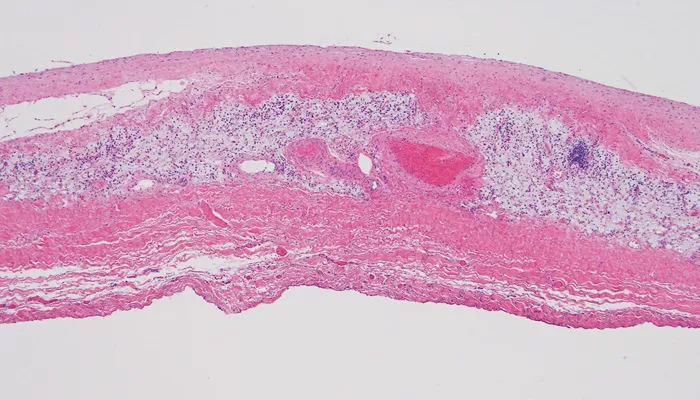
Pericarditis Imaging: In some cases, an echocardiogram (ultrasound of the heart) may be used to evaluate pericarditis.
Pericardial effusion, which is fluid buildup around the heart, is a common finding in pericarditis. Additionally, a chest X-ray may show an enlarged heart if there is significant fluid accumulation.
MI Imaging: In contrast, imaging for MI usually involves echocardiography to assess heart function and may show areas of wall motion abnormality in the region affected by the infarction. A coronary angiogram can directly visualize blockages in the coronary arteries, which is critical in diagnosing MI.
Other Clinical Features
Pericarditis: Patients with pericarditis often have a pericardial friction rub, a specific sound heard when listening to the chest with a stethoscope. This sound is caused by the inflamed pericardial layers rubbing together. It is an important diagnostic clue. Additionally, fever is common in viral and bacterial forms of pericarditis.
MI: In contrast, MI is often associated with symptoms of shock, including low blood pressure and a rapid, weak pulse. The patient may also experience cold sweats, nausea, and vomiting.
Treatment Approaches for Pericarditis and MI
The treatment for pericarditis and MI is very different, reflecting the distinct causes and mechanisms of the two conditions.
Pericarditis Treatment
Treatment for pericarditis typically includes:
Anti-inflammatory medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or aspirin, are commonly used to reduce inflammation and relieve pain.
Colchicine: This medication is often used to reduce the recurrence of pericarditis.
Corticosteroids: In certain cases, particularly in patients with autoimmune causes, corticosteroids may be prescribed.
Treatment of underlying causes: If pericarditis is due to an infection, antibiotics or antiviral medications may be necessary.
MI Treatment
The primary goal in the treatment of myocardial infarction is to restore blood flow to the affected area of the heart. Key treatments include:
Aspirin and Antiplatelet drugs: These help to prevent further clotting in the coronary arteries.
Thrombolytics: If the MI is caused by a clot, thrombolytic drugs may be administered to dissolve the clot.
Percutaneous Coronary Intervention (PCI): In many cases, PCI is performed to open blocked coronary arteries using a catheter and stent.
Coronary Artery Bypass Grafting (CABG): For severe blockages, CABG surgery may be necessary to bypass the affected coronary arteries.
Conclusion
Differentiating between pericarditis and myocardial infarction is critical in providing the correct treatment for patients.
While both conditions can present with chest pain, the clinical presentation, diagnostic findings, and treatment approaches vary significantly. An ECG, blood tests, and imaging studies can help healthcare providers distinguish between the two conditions. By understanding these differences, clinicians can ensure that patients receive the most appropriate and effective care.
Related topics: