Supraventricular Tachycardia (SVT) is a fast-paced heart rhythm disorder originating above the heart’s ventricles. It can cause a rapid heartbeat, leading to significant health concerns if not properly managed. Although many cases of SVT are benign and may not require emergency treatment, there are instances when SVT can be life-threatening. Understanding when SVT is an emergency is crucial for timely intervention and preventing complications. This article will delve into the key factors that determine when SVT becomes an emergency, the symptoms to watch for, and the appropriate treatment options.
What Is Supraventricular Tachycardia (SVT)?
Supraventricular Tachycardia refers to a group of arrhythmias where the heart’s atria or the atrioventricular (AV) node cause the heart to beat unusually fast. The heart rate typically exceeds 100 beats per minute, often reaching 150-250 beats per minute. The condition occurs due to an electrical malfunction that causes the heart to beat too quickly, disrupting its normal rhythm. SVT can arise from various conditions, including atrial fibrillation, atrial flutter, and other types of arrhythmias.
While many cases of SVT are not life-threatening, they can still cause discomfort and may lead to more severe cardiovascular issues if not treated in a timely manner.
Recognizing the Symptoms of SVT
Recognizing the symptoms of SVT is essential for determining when medical intervention is needed. Some common symptoms of SVT include:
Palpitations: A feeling of rapid or irregular heartbeats.
Dizziness or Lightheadedness: SVT can lead to a decrease in blood flow to the brain, causing dizziness.
Chest Pain: Some individuals may experience chest discomfort, which may be a sign of reduced blood flow to the heart.
Shortness of Breath: Difficulty breathing is common with SVT due to the increased demand on the heart.
Fatigue: A feeling of unusual tiredness or weakness.
In some cases, SVT may occur without noticeable symptoms, or the symptoms may resolve on their own, especially in the case of paroxysmal SVT (a type that starts and ends suddenly). However, if the condition lasts for an extended period or worsens, it can become a medical emergency.
When Is SVT An Emergency?
Not all cases of SVT require immediate medical attention, but several factors can make SVT an emergency. These include:
1. Prolonged or Persistent SVT
One of the most common triggers for emergency intervention is when SVT lasts for an extended period. If an SVT episode lasts for more than 30 minutes, it can lead to serious complications. Prolonged episodes may cause significant strain on the heart, resulting in a decrease in cardiac efficiency. In severe cases, this can lead to congestive heart failure or even a stroke.
2. Associated with Severe Symptoms
If an SVT episode is accompanied by severe symptoms, such as chest pain, shortness of breath, fainting, or significant dizziness, it is considered an emergency. These symptoms may indicate that the heart is not pumping effectively, potentially leading to further complications such as heart attack or stroke.
3. SVT in People with Preexisting Heart Disease
Individuals who already have underlying heart conditions, such as coronary artery disease, heart failure, or previous heart attacks, may be at greater risk when experiencing SVT. In these patients, the fast heart rate can exacerbate the preexisting condition, increasing the risk of a life-threatening event like a myocardial infarction (heart attack).
Therefore, SVT in individuals with heart disease warrants urgent medical attention.
4. SVT with Hemodynamic Instability
SVT can sometimes cause hemodynamic instability, where the heart’s ability to pump blood effectively is impaired. This is especially concerning if there is a drop in blood pressure or if the person becomes faint or loses consciousness. Hemodynamic instability is a clear indicator of an emergency, as it can lead to shock or organ failure.
5. SVT in the Presence of Other Medical Conditions
SVT may become more dangerous if the patient has other medical conditions such as hypertension (high blood pressure), diabetes, or thyroid disorders. These conditions can exacerbate the effects of SVT, increasing the likelihood of serious complications like heart failure or stroke. Additionally, in elderly patients, the risk of complications from SVT is higher, making it crucial to address the condition promptly.
Diagnosing SVT in Emergency Situations
When an individual presents with symptoms of SVT, a thorough evaluation is necessary to determine if the condition is an emergency.
The following diagnostic methods are commonly used:
Electrocardiogram (ECG)
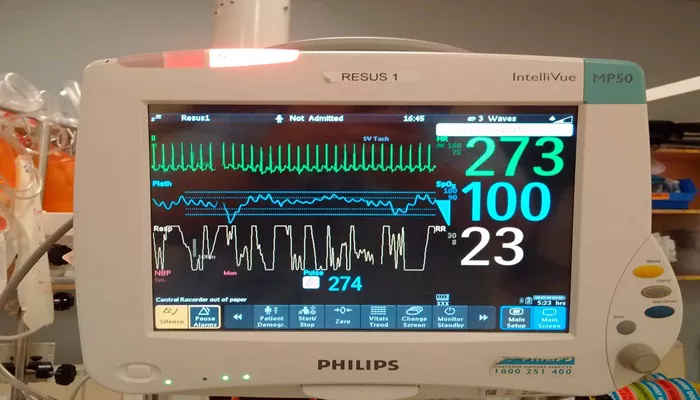
The primary diagnostic tool for SVT is the Electrocardiogram (ECG), which records the electrical activity of the heart.
During an episode of SVT, the ECG will show a rapid, regular heart rate originating above the ventricles. This helps doctors differentiate SVT from other types of arrhythmias, such as ventricular tachycardia, which can be more dangerous.
Blood Tests
Blood tests may be performed to check for electrolyte imbalances, thyroid dysfunction, or other conditions that could contribute to the development of SVT. Elevated thyroid levels, for example, may indicate hyperthyroidism, which can trigger arrhythmias.
Echocardiogram
An echocardiogram is an ultrasound of the heart that can assess the heart’s structure and function. It can help determine if there is any underlying heart disease contributing to the SVT episode.
Holter Monitor
In cases of recurrent SVT, a Holter monitor may be used to track the heart’s electrical activity over an extended period. This device records the heart’s rhythm continuously for 24-48 hours, allowing doctors to identify patterns that may indicate when SVT is most likely to occur.
Treatment Options for Emergency SVT
If SVT is deemed an emergency, prompt treatment is required to restore a normal heart rhythm and prevent complications.
Treatment options include:
Vagal Maneuvers
For individuals with paroxysmal SVT (which comes and goes), vagal maneuvers may be effective in slowing the heart rate.
These maneuvers include actions such as holding your breath and bearing down (Valsalva maneuver), coughing, or placing an ice pack on the face. These techniques stimulate the vagus nerve, which can help regulate the heart’s electrical signals.
Medications
In cases where vagal maneuvers do not work or the symptoms are severe, medications may be administered to slow the heart rate.
Common medications for SVT include adenosine, a drug that temporarily blocks the electrical signals in the heart to reset the rhythm, and beta-blockers or calcium channel blockers, which help to reduce the heart rate.
Cardioversion
If SVT persists or is associated with dangerous symptoms, cardioversion may be required. This procedure involves delivering a controlled electric shock to the heart to restore a normal rhythm.
Cardioversion is typically performed under sedation to minimize discomfort.
Catheter Ablation
In cases of recurrent or persistent SVT, catheter ablation may be recommended as a long-term treatment. During this procedure, a catheter is inserted into the heart, and areas of abnormal electrical tissue are destroyed using radiofrequency energy. This treatment can help prevent future SVT episodes and may be considered in patients who do not respond to medications.
Conclusion
Supraventricular Tachycardia (SVT) can be a serious condition, especially when it leads to severe symptoms or complications. While not all cases of SVT require emergency treatment, it is important to recognize the signs that indicate when immediate medical attention is needed. If you or someone you know experiences prolonged or severe symptoms of SVT, it is crucial to seek medical help as soon as possible.
Related topics: