Atrial contraction plays a key role in the functioning of the heart. It ensures that blood is efficiently pushed into the ventricles, which are responsible for pumping blood to the lungs and the rest of the body. In this article, we will break down the process of atrial contraction, starting from the electrical signals that trigger it to the mechanical events that follow.
Introduction to Atrial Contraction
The heart consists of four chambers: two atria (upper chambers) and two ventricles (lower chambers). The heart’s pumping action is divided into two phases: diastole and systole. During systole, the heart contracts to pump blood, while during diastole, it relaxes to allow blood to flow in. Atrial contraction happens during the latter stages of diastole, just before the ventricles contract.
Atrial contraction is an essential process for filling the ventricles with blood. This phase, sometimes called “atrial kick,” helps to optimize the volume of blood pumped by the heart, particularly during conditions like exercise or high blood demand.
The Electrical Mechanism Behind Atrial Contraction
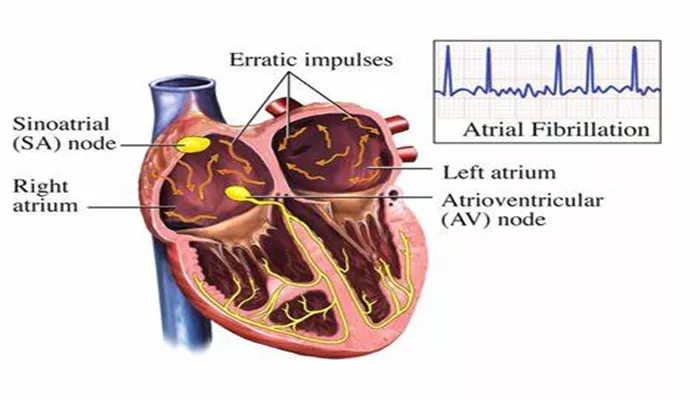
The process of atrial contraction is driven by electrical impulses. The heart has a natural pacemaker, the sinoatrial (SA) node, located in the right atrium. This node generates electrical impulses that regulate the heart’s rhythm.
1. Generation of the Electrical Impulse by the SA Node
The SA node is the primary pacemaker of the heart. It sends out electrical signals to both atria, causing them to contract.
The electrical impulses are generated spontaneously, and they spread across the atria, initiating the depolarization of the atrial muscle cells.
2. Impulse Propagation and Atrial Depolarization
Once the electrical impulse leaves the SA node, it travels through the right atrium to the left atrium via the Bachmann’s bundle, a specialized bundle of conducting fibers. As the electrical signal reaches the atrial muscle cells, it triggers the process of depolarization.
Atrial depolarization results in the contraction of the atrial muscles.
This contraction is essential for pushing the remaining blood from the atria into the ventricles, particularly the right ventricle in the case of the right atrium, and the left ventricle in the case of the left atrium.
The Role of the Atrioventricular (AV) Node
After the electrical impulse causes atrial depolarization, it passes through the atrioventricular (AV) node. The AV node acts as a gatekeeper, delaying the transmission of the impulse to the ventricles.
This delay ensures that the atria have enough time to contract fully and empty their contents into the ventricles before the ventricles contract.
The delay is crucial because it allows for a smooth and coordinated contraction of the heart. If this delay were too short or too long, the efficiency of the heart’s pumping action would be compromised.
Atrial Contraction and Its Effect on the Ventricles
The mechanical contraction of the atria is critical in ensuring that the ventricles receive enough blood before they contract.
When the atria contract, they force the remaining blood from the atria into the ventricles.
1. Ventricular Filling
The ventricular filling process occurs in two stages. First, blood flows passively into the ventricles when they are relaxed.
Then, during atrial contraction, the atria provide an additional “kick,” pushing the remaining blood into the ventricles. This is the atrial kick, which accounts for approximately 20-30% of the total ventricular filling, depending on heart rate and other factors.
2. Importance of the Atrial Kick
The atrial kick is particularly important during exercise or times of increased demand. During these times, the heart rate increases, and the time available for ventricular filling decreases. The atrial contraction ensures that the ventricles receive enough blood to pump efficiently, meeting the increased oxygen demand of the body.
Factors Affecting Atrial Contraction
Several factors can influence the effectiveness of atrial contraction, and ultimately, the heart’s ability to pump blood effectively.
1. Heart Rate
As the heart rate increases, the time between beats shortens. This can reduce the time available for ventricular filling and decrease the contribution of the atrial kick. In high heart rate conditions, such as during exercise, the atrial contraction becomes even more important for maintaining optimal ventricular filling.
2. Atrial Arrhythmias
Conditions like atrial fibrillation or atrial flutter can disrupt normal atrial contraction. In atrial fibrillation, the atria do not contract effectively, and blood flow to the ventricles becomes less coordinated. This can lead to decreased cardiac output and increased risk for stroke due to the formation of blood clots.
3. Cardiac Diseases
Certain cardiac conditions, such as hypertrophy (thickening of the heart muscle) or heart failure, can impair the atrial contraction process. In these cases, the atria may become less effective at pushing blood into the ventricles, and this can compromise the overall efficiency of the heart.
Conclusion
Atrial contraction is a vital part of the heart’s overall function, ensuring that the ventricles are filled with enough blood before they contract. This mechanical action, driven by electrical impulses from the SA node and coordinated by the AV node, is essential for efficient blood flow and cardiovascular health.
Understanding how atrial contraction occurs provides insights into many common heart conditions and the importance of maintaining a healthy heart. When atrial contraction is compromised, it can lead to significant cardiovascular complications, making its study a critical aspect of cardiology.
Related topics: