Atrial tachycardia (AT) is a condition where the heart’s upper chambers (atria) beat faster than normal. The atria’s electrical system becomes disrupted, causing the heart to beat rapidly and irregularly. This leads to a variety of symptoms such as palpitations, dizziness, shortness of breath, and in some cases, fainting. Atrial tachycardia can occur in people of all ages, though it is more commonly seen in those with heart disease or structural abnormalities.
Understanding the types of atrial tachycardia is crucial for diagnosis and treatment. There are two primary types of atrial tachycardia: focal atrial tachycardia (FAT) and multi-focal atrial tachycardia (MAT). Both types result in an abnormal increase in heart rate, but the causes, symptoms, and treatments can differ. This article provides an overview of these two types, exploring their causes, mechanisms, diagnostic methods, and treatment options.
Focal Atrial Tachycardia (FAT)
Overview
Focal atrial tachycardia (FAT) is the most common type of atrial tachycardia. It occurs when a single area or “focus” of the atrium starts to fire electrical signals rapidly. This focus becomes the abnormal pacemaker of the heart, overriding the heart’s natural pacemaker (the sinoatrial node). As a result, the heart rate increases, typically between 100 to 250 beats per minute.
Causes and Mechanisms
Focal atrial tachycardia can be caused by several factors:
Structural heart disease: Conditions like atrial fibrosis, atrial enlargement, or scar tissue in the atrium due to previous heart surgeries or heart attacks may create abnormal electrical circuits.
Idiopathic cases: In some instances, no underlying heart disease is found. These cases are referred to as “idiopathic” FAT and can occur in otherwise healthy individuals.
Electrophysiological disturbances: In certain cases, abnormal tissue in the atria can trigger rapid electrical impulses.
These tissues may act as a secondary pacemaker, initiating premature heartbeats that set off a rapid heart rate.
Focal atrial tachycardia usually originates in one of the atrial regions, most often the right atrium near the pulmonary veins, though it can also occur in the left atrium.
Symptoms
The symptoms of FAT include:
- Rapid heart rate (tachycardia)
- Palpitations (a sensation of a fast or irregular heartbeat)
- Dizziness or lightheadedness
- Shortness of breath
- Fatigue or weakness
In some cases, focal atrial tachycardia may be asymptomatic, meaning a person might not notice any symptoms but could still experience complications.
Diagnosis
To diagnose focal atrial tachycardia, doctors rely on:
Electrocardiogram (ECG): This test records the electrical activity of the heart and can show a rapid, regular rhythm with abnormal P waves, which are characteristic of FAT.
Holter monitoring: This is a continuous 24-hour ECG that can capture any abnormal rhythms that might not show up during a standard ECG.
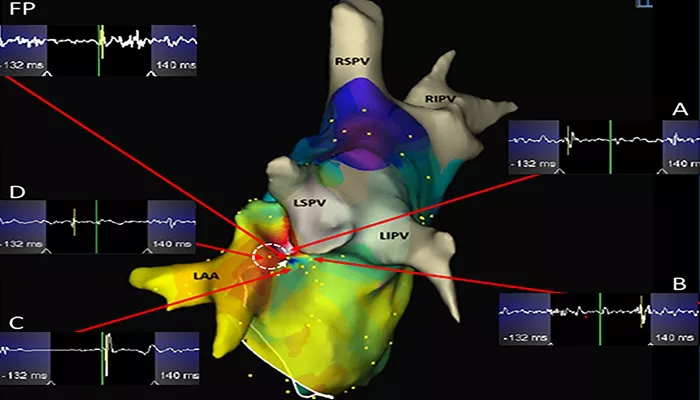
Electrophysiological study (EPS): In certain cases, a more detailed study of the heart’s electrical pathways is necessary.
This invasive test helps locate the specific area of abnormal electrical activity in the heart.
Treatment
Treatment of FAT aims to control the heart rate and prevent complications such as stroke or heart failure. Treatment options include:
Medications: Beta-blockers, calcium channel blockers, and antiarrhythmic drugs can be used to control the heart rate and rhythm.
Catheter ablation: In many cases, FAT can be treated with catheter ablation, a procedure where a catheter is inserted through the blood vessels to the heart to destroy the abnormal electrical tissue that causes the tachycardia.
Electrical cardioversion: If the heart rate is extremely fast and unresponsive to medications, a controlled shock may be delivered to reset the heart’s rhythm.
Multi-Focal Atrial Tachycardia (MAT)
Overview
Multi-focal atrial tachycardia (MAT) is a less common type of atrial tachycardia, characterized by multiple areas within the atrium generating abnormal electrical signals. Unlike FAT, which originates from a single focus, MAT is marked by the presence of at least three different ectopic foci (abnormal areas of electrical activity) within the atrium. These foci cause the atria to contract rapidly and irregularly.
Causes and Mechanisms
MAT is often associated with underlying conditions that affect the atrium’s ability to maintain normal electrical conduction, including:
Chronic lung disease (COPD): This is one of the most common causes of MAT, particularly in patients with advanced COPD.
The changes in lung function can alter the electrical properties of the atria, leading to abnormal rhythms.
Electrolyte imbalances: High or low levels of potassium, magnesium, or calcium can disrupt the normal electrical conduction in the heart, triggering MAT.
Heart disease: Conditions such as heart failure or atrial fibrillation can increase the risk of developing MAT.
Alcohol use or drug abuse: Both alcohol and certain drugs can trigger abnormal electrical activity in the heart, leading to MAT.
MAT results in an irregular, often rapid heart rate. The presence of multiple ectopic foci means that the electrical activity is more erratic compared to focal atrial tachycardia.
Symptoms
The symptoms of MAT are similar to those of other types of atrial tachycardia:
- Rapid heart rate and palpitations
- Shortness of breath
- Fatigue and dizziness
- Chest discomfort in some cases
MAT may also lead to poor circulation, causing lightheadedness and fainting in some individuals, especially during episodes of rapid tachycardia.
Diagnosis
Diagnosing multi-focal atrial tachycardia involves:
Electrocardiogram (ECG): An ECG will show irregular P waves originating from multiple foci. The rhythm is often highly irregular, and the P waves will vary in appearance.
Holter monitoring: A 24-hour Holter monitor can capture episodes of MAT, especially if they occur intermittently.
Electrophysiological study: In some cases, an EPS can help map the multiple abnormal electrical foci in the atrium, although this is less commonly required for MAT.
Treatment
The treatment of MAT focuses on controlling the heart rate and addressing the underlying causes. Key treatment options include:
Managing underlying conditions: The first step in treating MAT is to manage any underlying conditions, such as chronic lung disease, heart failure, or electrolyte imbalances.
Medications: Rate-controlling medications such as beta-blockers or calcium channel blockers can help reduce the heart rate and alleviate symptoms. Antiarrhythmic medications may also be used in some cases.
Oxygen therapy: In patients with COPD or other lung diseases, supplemental oxygen may help reduce the frequency of MAT episodes.
Catheter ablation: In some cases, catheter ablation may be considered, although this is less common than for focal atrial tachycardia. The presence of multiple ectopic foci can make ablation more challenging.
Conclusion
Atrial tachycardia is a condition that can significantly affect an individual’s quality of life, but it is treatable. The two primary types—focal atrial tachycardia (FAT) and multi-focal atrial tachycardia (MAT)—differ in their origins, causes, and treatment approaches. FAT is typically caused by a single abnormal electrical focus, while MAT is marked by multiple ectopic foci. Both types can be managed effectively with medications and, in many cases, catheter ablation.
Related topics: