Heart failure (HF) is a complex condition where the heart is unable to pump blood effectively, leading to inadequate tissue perfusion and oxygenation. Patients with heart failure often experience arrhythmias, or irregular heartbeats, which can worsen the symptoms of heart failure and complicate treatment. Antiarrhythmic drugs are frequently used to manage these arrhythmias. However, not all antiarrhythmic medications are safe for individuals with heart failure. Some of these drugs can have harmful effects, exacerbating heart failure symptoms and increasing the risk of mortality.
This article will discuss which antiarrhythmics are contraindicated in heart failure, highlighting the mechanisms that make these drugs unsafe for heart failure patients. We will also explore alternative medications and strategies for managing arrhythmias in heart failure patients.
Understanding The Link Between Heart Failure And Arrhythmias
Heart failure is often associated with a higher risk of arrhythmias due to structural and electrical remodeling of the heart.
This includes changes such as enlargement of the heart chambers, fibrosis, and alterations in ion channel function.
Arrhythmias commonly encountered in heart failure include atrial fibrillation (AF), ventricular tachycardia (VT), and atrial flutter.
Arrhythmias can worsen the symptoms of heart failure, including shortness of breath, fatigue, and fluid retention. In some cases, arrhythmias can lead to sudden cardiac death if left untreated. Antiarrhythmic drugs help restore normal rhythm and control arrhythmias, but their use must be carefully managed in heart failure patients due to potential risks.
Antiarrhythmic Drugs and Their Mechanisms
Antiarrhythmic drugs are categorized into four classes based on their mechanisms of action:
Class I: Sodium channel blockers, which include subgroups IA, IB, and IC.
Class II: Beta-blockers, which reduce the effects of adrenaline on the heart.
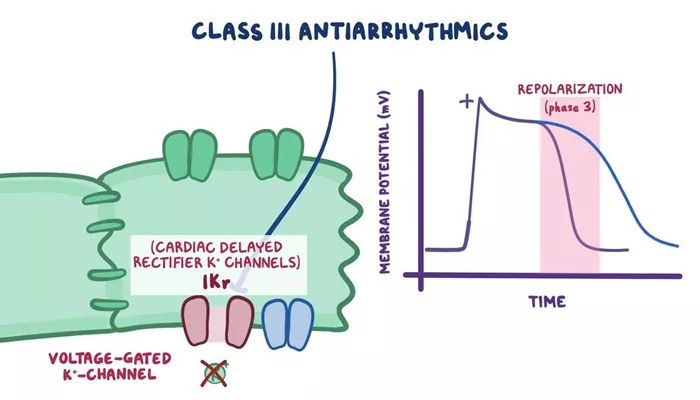
Class III: Potassium channel blockers, which prolong the action potential duration.
Class IV: Calcium channel blockers, which inhibit calcium influx into cells.
While some of these drugs can be effective for treating arrhythmias, others are contraindicated in patients with heart failure due to their proarrhythmic effects or negative impact on heart function.
Class I Antiarrhythmics (Sodium Channel Blockers)
Class I antiarrhythmics include several drugs that block sodium channels, which slows down the electrical conduction in the heart.
They are further divided into three subgroups:
Class IA (e.g., Quinidine, Procainamide, Disopyramide): These drugs prolong the action potential and can be used to treat atrial fibrillation, atrial flutter, and ventricular arrhythmias. However, they are generally contraindicated in heart failure. For example, Disopyramide, a potent sodium channel blocker, is known to depress contractility and can worsen heart failure symptoms by reducing myocardial contractility and increasing the risk of arrhythmias.
Class IB (e.g., Lidocaine, Mexiletine): These drugs have a mild effect on sodium channels and are mainly used in ventricular arrhythmias.
Lidocaine, for example, is frequently used in emergency settings to treat ventricular arrhythmias. While generally safer in patients with heart failure than Class IA drugs, Lidocaine should still be used cautiously, particularly in severe heart failure, as it can cause hypotension and further depress myocardial function in high doses.
Class IC (e.g., Flecainide, Propafenone): Flecainide and Propafenone are potent sodium channel blockers, and while they are effective for treating atrial arrhythmias, they are contraindicated in heart failure due to their potential to increase the risk of mortality. Both drugs have been shown to exacerbate heart failure by reducing myocardial contractility and increasing the risk of ventricular arrhythmias. In heart failure, the weakened heart muscle is more vulnerable to proarrhythmic effects, and these medications can worsen symptoms or lead to fatal arrhythmias.
Class II Antiarrhythmics (Beta-Blockers)
Beta-blockers are commonly used in heart failure management to reduce heart rate, lower blood pressure, and improve left ventricular function. In fact, several beta-blockers (e.g., Carvedilol, Metoprolol, and Bisoprolol) have been proven to reduce mortality and morbidity in heart failure patients.
However, beta-blockers should not be confused with antiarrhythmic agents in the traditional sense. While beta-blockers act to reduce arrhythmias by blocking the effects of adrenaline, they are usually well-tolerated in heart failure patients, especially those with systolic dysfunction. But careful monitoring is still necessary, particularly during dose escalation, as excessive beta-blockade can exacerbate symptoms in heart failure patients, causing bradycardia or worsening hypotension.
In some cases, non-selective beta-blockers (e.g., Propranolol) are avoided due to their potential to cause more pronounced negative effects on heart failure, but Cardioselective beta-blockers (like Metoprolol succinate) are often the first-line treatment.
Class III Antiarrhythmics (Potassium Channel Blockers)
Class III antiarrhythmics, such as Amiodarone, Dofetilide, and Sotalol, work by blocking potassium channels, which prolong the repolarization phase of the action potential and help to restore normal rhythm. While these drugs are often used in heart failure patients to control arrhythmias, some of them have specific contraindications or require cautious use:
Amiodarone: Amiodarone is one of the most widely used antiarrhythmics in patients with heart failure, as it has been shown to be relatively safe in treating both atrial and ventricular arrhythmias in heart failure. However, its use can be associated with significant side effects, including thyroid dysfunction, pulmonary fibrosis, and liver toxicity, which require close monitoring. Despite these risks, it is often preferred over other antiarrhythmics in heart failure due to its relatively favorable safety profile.
Dofetilide: This drug is effective in treating atrial fibrillation and atrial flutter, but it is contraindicated in patients with severe renal dysfunction or QT prolongation, conditions that are often seen in advanced heart failure. Dofetilide can increase the risk of torsades de pointes, a potentially life-threatening arrhythmia, and its use should be carefully monitored with frequent ECGs.
Sotalol: While Sotalol is a combined beta-blocker and potassium channel blocker, it is contraindicated in heart failure patients with severe left ventricular dysfunction. Sotalol can worsen heart failure by reducing myocardial contractility, leading to further deterioration of cardiac function.
Class IV Antiarrhythmics (Calcium Channel Blockers)
Class IV antiarrhythmics include Verapamil and Diltiazem, both of which block calcium channels and are used to treat atrial fibrillation and atrial flutter. While these medications can be effective at controlling heart rate, they are contraindicated in heart failure with reduced ejection fraction (HFrEF).
The use of Verapamil and Diltiazem in patients with HFrEF can worsen heart failure symptoms by decreasing myocardial contractility and impairing conduction through the atrioventricular (AV) node. These medications can also exacerbate hypotension and lead to bradycardia, further impairing cardiac output.
Alternatives for Managing Arrhythmias in Heart Failure
In patients with heart failure, the management of arrhythmias requires careful consideration of the underlying cardiac dysfunction and the potential impact of antiarrhythmic therapy. Some alternative strategies include:
Device Therapy: Implantable cardioverter-defibrillators (ICDs) are used in patients with heart failure at high risk for life-threatening arrhythmias, such as ventricular tachycardia or ventricular fibrillation.
Catheter Ablation: For patients with atrial fibrillation or other arrhythmias, catheter ablation may be considered, especially in those who are intolerant to antiarrhythmic medications.
Rate Control with Beta-Blockers: As previously mentioned, beta-blockers (like Carvedilol) are often the first line of treatment for rate control in heart failure patients with atrial fibrillation.
Conclusion
While antiarrhythmic medications are essential in treating arrhythmias in heart failure patients, some of these drugs can have detrimental effects on cardiac function and exacerbate heart failure. It is crucial to carefully select and monitor the use of antiarrhythmic drugs, considering their potential side effects and contraindications in heart failure. Class I drugs, particularly those in the IC subgroup, as well as certain potassium channel blockers and calcium channel blockers, should generally be avoided in heart failure patients. On the other hand, beta-blockers, amiodarone, and other therapies may be more appropriate for managing arrhythmias without compromising heart function.
Related topics: