Paroxysmal tachycardia (PT) refers to an episode of rapid heart rate that begins and ends suddenly, typically without warning. It is usually caused by a malfunction in the electrical system of the heart, which can lead to the heart beating faster than normal. The rate can range from 100 to 300 beats per minute (bpm), and episodes can last from a few seconds to several hours. This condition can be distressing and uncomfortable for individuals who experience it, often causing symptoms like dizziness, palpitations, chest discomfort, and in some cases, fainting.
There are different types of paroxysmal tachycardia, but the most common include atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT), and focal atrial tachycardia (FAT). Treatment options vary depending on the specific type and severity of the tachycardia, but the primary goal is to terminate the episode and prevent further recurrences. One of the key aspects of managing paroxysmal tachycardia is pharmacological intervention.
This article will explore the drug of choice for paroxysmal tachycardia, the mechanisms behind its effectiveness, and considerations for its use in clinical practice.
Understanding Paroxysmal Tachycardia
Before diving into the pharmacological treatments, it is essential to understand the nature of paroxysmal tachycardia. The term “paroxysmal” means that the tachycardia (or rapid heart rate) begins suddenly and can resolve just as quickly. The condition is often intermittent and can occur sporadically in patients with underlying heart disease or even in those with no previous cardiac issues.
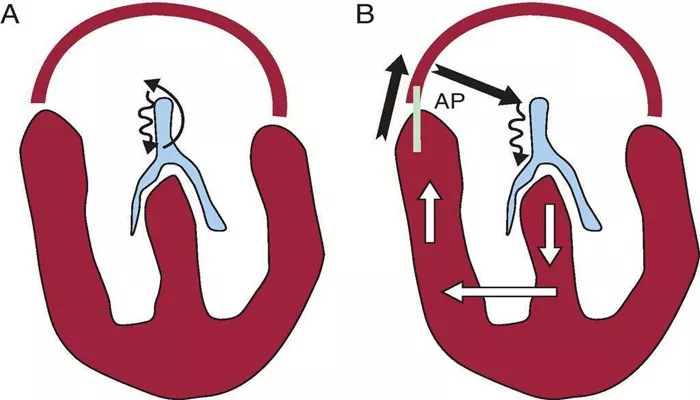
Paroxysmal tachycardia occurs due to abnormal electrical impulses in the heart, which can cause the heart to beat irregularly and faster than usual. The heart’s electrical conduction system, which includes the sinoatrial (SA) node, atrioventricular (AV) node, and the His-Purkinje system, is responsible for regulating the timing of each heartbeat. In paroxysmal tachycardia, these electrical impulses can become aberrant, leading to rapid and abnormal heartbeats.
Symptoms of Paroxysmal Tachycardia
The symptoms of paroxysmal tachycardia can vary, but common signs and symptoms include:
Palpitations: An awareness of a fast or irregular heartbeat.
Dizziness: Due to reduced blood flow to the brain during rapid heart rhythms.
Chest discomfort or pain: Can be mild or severe, resembling angina.
Shortness of breath: Often associated with a rapid heartbeat, especially during physical activity.
Fainting or near-fainting: Due to a lack of adequate blood flow to vital organs.
These symptoms can occur suddenly and without warning, often lasting for minutes to hours before resolving on their own or with intervention.
Pharmacological Treatment for Paroxysmal Tachycardia
There are several medications available to treat paroxysmal tachycardia, and the choice of drug largely depends on the type of tachycardia and its underlying cause. The main goal of treatment is to terminate the tachycardia episode quickly and restore normal sinus rhythm (the normal rhythm of the heart).
The most common approach for managing paroxysmal tachycardia involves the use of antiarrhythmic drugs. These drugs help to control the electrical impulses in the heart, either by slowing down the heart rate or by terminating the abnormal rhythm altogether. Among the variety of drugs available, adenosine is typically considered the drug of choice for most types of paroxysmal tachycardia, especially in cases where the tachycardia is supraventricular.
Adenosine: The Drug of Choice for Paroxysmal Tachycardia
Adenosine is the primary drug used for the treatment of paroxysmal tachycardia. It is particularly effective for terminating supraventricular tachycardia (SVT), which is the most common type of paroxysmal tachycardia. Supraventricular tachycardia arises from the atria or the AV node, and it is typically characterized by a rapid, regular heart rate.
Mechanism of Action
Adenosine works by affecting the AV node, which is the electrical junction between the atria and the ventricles of the heart.
The drug slows down electrical conduction through the AV node, which can interrupt the abnormal electrical circuits responsible for the tachycardia. By halting the electrical impulses for a brief moment, adenosine allows the heart to reset itself and return to a normal rhythm. This sudden interruption of electrical activity is called “transient AV block.”
Adenosine’s effect is very short-lived—lasting only a few seconds—so the heart usually resumes a normal rhythm after the drug is administered. This makes it highly effective in acute settings and in emergency care situations, as it can quickly terminate a tachycardia episode.
Administration
Adenosine is usually administered intravenously (IV) in a hospital setting. The typical dose is 6 mg, followed by a flush of saline to ensure that the drug reac
hes the heart rapidly. If the initial dose does not successfully terminate the tachycardia, a higher dose (usually 12 mg) can be given. The drug should always be administered by a trained healthcare provider, as it can cause transient side effects such as a feeling of chest pressure, shortness of breath, or even a brief period of asystole (absence of a heartbeat), which is generally not harmful but requires monitoring.
Effectiveness
Adenosine is highly effective for treating most forms of supraventricular tachycardia, with a success rate of around 90%. It is particularly useful for treating conditions like AVNRT and AVRT, which are common causes of paroxysmal tachycardia.
However, it is not effective for ventricular tachycardia or other types of arrhythmias originating from the ventricles.
Alternatives to Adenosine
While adenosine is often the first-line treatment for paroxysmal tachycardia, there are other drugs and interventions that may be used if adenosine is ineffective or inappropriate. These include:
Calcium Channel Blockers (e.g., Verapamil or Diltiazem): These medications can be used for the management of paroxysmal tachycardia, particularly when the tachycardia originates in the atria.
They work by inhibiting calcium entry into the heart muscle, which slows the heart rate and stabilizes the electrical conduction system.
Beta-Blockers (e.g., Metoprolol or Esmolol): Beta-blockers can help reduce heart rate and are sometimes used for tachycardia that is not immediately responsive to adenosine. They work by blocking the beta-adrenergic receptors, which reduces the effects of adrenaline and slows the heart rate.
Antiarrhythmic Drugs (e.g., Flecainide or Propafenone): These drugs are often used for more persistent or recurrent cases of paroxysmal tachycardia. They work by stabilizing the electrical activity in the heart and preventing the abnormal circuits that cause tachycardia.
When Is Adenosine Not Recommended?
Although adenosine is generally considered safe, there are certain situations where it may not be the best option. These include:
Severe Asthma: Adenosine can cause bronchoconstriction, which may worsen asthma symptoms in some patients.
Second- or Third-Degree Heart Block: Since adenosine works by slowing conduction through the AV node, it may worsen heart block in patients with preexisting conduction abnormalities.
Ventricular Tachycardia: Adenosine is not effective for treating ventricular tachycardia, and its use in such cases could be harmful. If ventricular tachycardia is suspected, alternative treatments are needed.
Conclusion
In the treatment of paroxysmal tachycardia, the drug of choice is typically adenosine. It is highly effective for managing supraventricular tachycardias, particularly AVNRT and AVRT, by temporarily interrupting the abnormal electrical circuits and allowing the heart to return to its normal rhythm. Although adenosine is the first-line treatment in most cases, alternative medications such as calcium channel blockers, beta-blockers, or antiarrhythmic drugs may be considered when adenosine is ineffective or inappropriate.
Related topics: