Hypercholesterolemia, or high cholesterol, is a condition in which there are elevated levels of cholesterol in the blood.
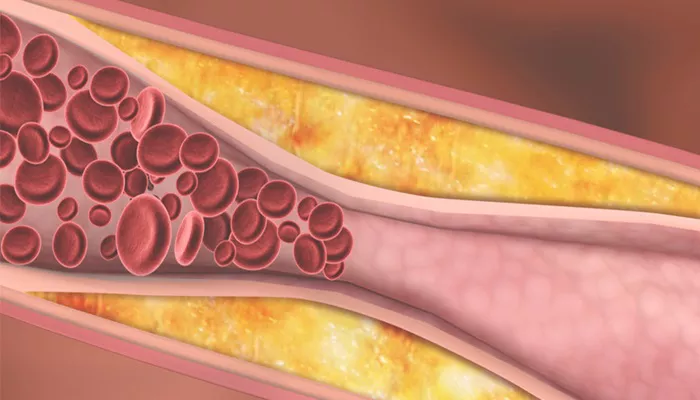
Cholesterol is a waxy, fat-like substance that is necessary for building cell membranes, producing certain hormones, and aiding in digestion. However, excessive amounts can lead to plaque buildup in the arteries, increasing the risk for cardiovascular diseases such as heart attacks and strokes.
Diagnosing hypercholesterolemia involves identifying abnormal cholesterol levels through various methods, primarily blood tests. Early diagnosis is crucial since hypercholesterolemia often doesn’t show symptoms until significant damage has already occurred to the arteries. This article will explore how hypercholesterolemia is diagnosed, including the types of tests used, the interpretation of results, and how healthcare providers use this information to develop treatment plans.
The Role of Cholesterol in the Body
Before diving into the diagnostic methods, it is essential to understand what cholesterol is and why its levels matter.
Cholesterol is carried through the bloodstream by two main types of lipoproteins: low-density lipoprotein (LDL) and high-density lipoprotein (HDL). LDL is often referred to as “bad” cholesterol because high levels can lead to plaque formation in the arteries. On the other hand, HDL is known as “good” cholesterol, as it helps remove excess cholesterol from the blood vessels and prevents plaque buildup.
When diagnosing hypercholesterolemia, healthcare providers are particularly concerned with the levels of LDL cholesterol, total cholesterol, and sometimes triglycerides, as they are critical indicators of cardiovascular health.
The Initial Consultation and Risk Assessment
The diagnostic process for hypercholesterolemia typically begins with a detailed consultation. Your healthcare provider will take a comprehensive health history, discussing lifestyle factors such as diet, exercise habits, and family medical history.
This helps identify individuals at higher risk of developing high cholesterol.
Several risk factors increase the likelihood of hypercholesterolemia, including:
Age: Cholesterol levels tend to rise as people get older.
Family history: A family history of high cholesterol or heart disease can predispose individuals to hypercholesterolemia.
Poor diet: Diets high in saturated fats and trans fats can contribute to higher cholesterol levels.
Lack of exercise: A sedentary lifestyle can lower HDL levels and raise LDL levels.
Other health conditions: Conditions like diabetes and hypothyroidism can also lead to higher cholesterol levels.
During this consultation, your healthcare provider will assess your overall cardiovascular risk to determine whether blood testing for cholesterol is necessary.
Blood Tests for Cholesterol Levels
The most common and definitive way to diagnose hypercholesterolemia is through blood tests that measure the different types of cholesterol in your blood. These tests include the lipid panel or lipid profile, which provides detailed information on cholesterol levels. The lipid panel is typically ordered after a physical examination and risk assessment.
1. Fasting Lipid Panel
A fasting lipid panel is the gold standard for diagnosing hypercholesterolemia. It measures several lipid components in the blood, including:
Total Cholesterol: This value represents the sum of all cholesterol types in the blood. Ideally, total cholesterol should be less than 200 mg/dL. Levels above 240 mg/dL are considered high.
Low-Density Lipoprotein (LDL): Often referred to as “bad” cholesterol, high levels of LDL can lead to plaque buildup in the arteries, causing atherosclerosis. Optimal LDL levels are below 100 mg/dL. Levels above 160 mg/dL are considered high.
High-Density Lipoprotein (HDL): Known as “good” cholesterol, HDL helps remove excess cholesterol from the bloodstream. Higher HDL levels are protective against heart disease. An HDL level of 60 mg/dL or higher is considered optimal, while levels below 40 mg/dL are a concern.
Triglycerides: These are another type of fat found in the blood. Elevated triglycerides are often associated with an increased risk of heart disease. Normal triglyceride levels are below 150 mg/dL.
A fasting lipid panel requires patients to fast for at least 8 hours before the blood draw to ensure the most accurate readings, particularly for triglycerides.
2. Non-Fasting Lipid Panel
In some cases, a non-fasting lipid panel may be performed. This type of test is more convenient because fasting is not required. However, it can produce slightly less accurate triglyceride measurements, which could lead to variations in the diagnosis. Non-fasting panels are usually ordered in follow-up visits or when fasting is not possible.
3. Advanced Lipid Testing
For patients with a higher risk of heart disease or those whose lipid panel results are difficult to interpret, advanced lipid testing may be performed. This can include:
Apolipoprotein B (ApoB): This protein is a component of LDL particles. A higher number of ApoB particles suggests a greater risk for cardiovascular disease.
Lipoprotein(a) or Lp(a): This test measures a specific type of LDL particle that may increase the risk of heart disease, particularly in individuals with a family history of premature heart disease.
Small Dense LDL Test: This test looks at the number of smaller, denser LDL particles, which are believed to be more harmful than larger LDL particles in terms of heart disease risk.
4. Home Cholesterol Testing Kits
In addition to blood tests performed in a medical setting, there are home cholesterol testing kits available. While they can provide a rough estimate of cholesterol levels, they are not as accurate as a professional lipid panel and should not be used for formal diagnosis. However, they can offer a starting point for individuals who wish to monitor their cholesterol at home.
How are the Results Interpreted?
After a blood test, your healthcare provider will interpret the results to determine if you have hypercholesterolemia.
Cholesterol levels are categorized into ranges to assess risk:
Total Cholesterol:
- Less than 200 mg/dL: Desirable
- 200–239 mg/dL: Borderline high
- 240 mg/dL or higher: High
LDL Cholesterol (Bad Cholesterol):
- Less than 100 mg/dL: Optimal
- 100–129 mg/dL: Near optimal
- 130–159 mg/dL: Borderline high
- 160–189 mg/dL: High
- 190 mg/dL or higher: Very high
HDL Cholesterol (Good Cholesterol):
- Less than 40 mg/dL: Low (major risk factor for heart disease)
- 40–59 mg/dL: Acceptable
- 60 mg/dL or higher: Optimal
Triglycerides:
- Less than 150 mg/dL: Normal
- 150–199 mg/dL: Borderline high
- 200–499 mg/dL: High
- 500 mg/dL or higher: Very high
If your cholesterol levels fall outside of the desirable range, it may indicate the need for further investigation. Your doctor will assess your cardiovascular risk, taking into account other factors like age, gender, smoking, blood pressure, and family history of heart disease.
Additional Tests for Accurate Diagnosis
In certain cases, your doctor may recommend additional tests to further evaluate your cardiovascular health, especially if lifestyle changes and medications do not seem effective in controlling cholesterol levels. These may include:
Carotid Ultrasound: An imaging test that uses sound waves to visualize the arteries in the neck. It helps determine if plaque is building up and the extent of any narrowing in the arteries.
Coronary Artery Calcium (CAC) Score: A test that uses a CT scan to detect calcium deposits in the coronary arteries. The higher the calcium score, the higher the risk of cardiovascular events.
Ankle-Brachial Index (ABI): A simple test that compares the blood pressure in your ankle to the blood pressure in your arm to assess the health of your arteries.
Conclusion
Diagnosing hypercholesterolemia is an essential step in preventing cardiovascular diseases. The primary diagnostic tool is a lipid panel, which measures the levels of LDL, HDL, total cholesterol, and triglycerides in the blood. By understanding these results and considering other risk factors, healthcare providers can assess an individual’s cardiovascular risk and create an appropriate treatment plan. If diagnosed early, lifestyle changes and medications can help manage cholesterol levels and reduce the risk of heart disease, stroke, and other serious conditions.
Related topics: