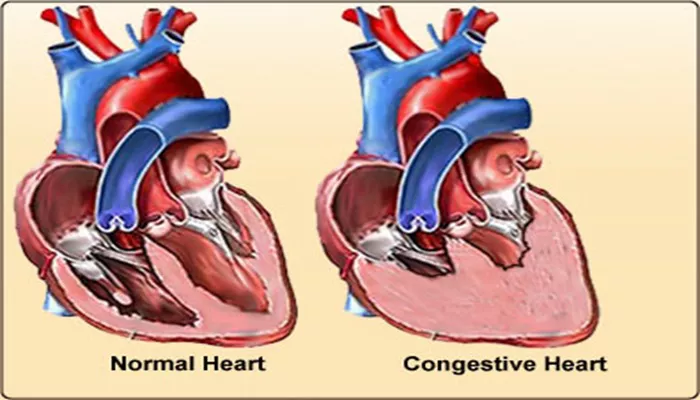
Congestive heart failure (CHF) is a condition where the heart is unable to pump blood effectively, leading to fluid accumulation in the lungs and other parts of the body. It is commonly associated with a range of physiological changes in the body, including an increase in hemoglobin levels. While it may seem counterintuitive at first, understanding the relationship between CHF and elevated hemoglobin levels requires a closer look at the body’s compensatory mechanisms.
This article aims to explain why hemoglobin levels may increase in individuals with CHF, the physiological processes behind it, and its implications for treatment and management.
What Is Hemoglobin?
Before diving into the specifics of CHF and hemoglobin, it’s essential to understand what hemoglobin is and its role in the body. Hemoglobin is a protein found in red blood cells, responsible for carrying oxygen from the lungs to tissues and returning carbon dioxide from tissues back to the lungs for exhalation. It plays a critical role in maintaining the body’s oxygen supply, which is vital for cellular function and overall health.
The Body’s Response to Low Oxygen in CHF
One of the primary mechanisms that link congestive heart failure and an increase in hemoglobin is the body’s response to low oxygen levels.
CHF reduces the heart’s ability to pump blood efficiently, leading to a reduced delivery of oxygenated blood to various organs and tissues.
As a result, the body may sense low oxygen levels (a condition known as hypoxia) and respond by attempting to compensate for this shortage.
The Role of Erythropoietin (EPO)
In response to hypoxia, the kidneys release a hormone called erythropoietin (EPO). EPO is a key regulator in the production of red blood cells. It stimulates the bone marrow to produce more red blood cells, thereby increasing hemoglobin levels.
This process is known as erythropoiesis. By increasing the number of red blood cells, the body attempts to improve its oxygen-carrying capacity to compensate for the reduced oxygen levels caused by CHF.
Chronic Hypoxia and Hemoglobin
In individuals with chronic heart failure, the body’s tissues are often in a state of low oxygen availability for extended periods. This persistent hypoxia leads to a more sustained release of EPO, which continually stimulates the bone marrow to produce red blood cells. Over time, this process can result in higher-than-normal hemoglobin levels, even if the individual is not in an acute state of hypoxia. This increase in hemoglobin is part of the body’s adaptive strategy to improve oxygen delivery.
Fluid Retention in CHF and Its Effect on Hemoglobin
Another factor contributing to the increase in hemoglobin in CHF is fluid retention. CHF often leads to fluid buildup in the body due to the heart’s inability to pump blood effectively. This excess fluid can cause dilution of blood, which might initially lower hemoglobin levels.
However, in response to this, the body might compensate by increasing erythropoiesis to counteract the dilution effect, resulting in a net increase in hemoglobin concentration.
Dehydration and Hemoconcentration
In some cases, individuals with CHF may experience dehydration due to factors such as inadequate fluid intake, diuretic use, or kidney dysfunction. Dehydration can lead to hemoconcentration, where the volume of plasma (the liquid component of blood) decreases, making the concentration of red blood cells, and thus hemoglobin, appear higher than normal. This hemoconcentration effect may also contribute to an increase in hemoglobin levels in certain individuals with CHF.
The Role of the Autonomic Nervous System
The autonomic nervous system, which regulates involuntary bodily functions, plays a significant role in CHF. In an attempt to compensate for reduced cardiac output, the body activates the sympathetic nervous system, which can lead to the release of various hormones that increase red blood cell production. This activation of the autonomic nervous system further amplifies the body’s efforts to boost hemoglobin levels.
Increased Erythropoiesis via Sympathetic Stimulation
In CHF, the activation of the sympathetic nervous system stimulates the release of catecholamines (such as adrenaline), which have been shown to enhance erythropoiesis. This process further contributes to the increased production of red blood cells and elevated hemoglobin levels.
The Effect of Renal Dysfunction in CHF
Renal dysfunction is common in individuals with congestive heart failure. The kidneys play a crucial role in regulating fluid balance and erythropoiesis through the release of erythropoietin. In CHF, kidney function can become impaired, leading to further complications, including an exaggerated release of erythropoietin. This dysfunction can lead to higher-than-normal levels of erythropoietin, resulting in an increase in hemoglobin and red blood cell production.
Impaired Oxygen Sensing in the Kidneys
In CHF, the kidneys may experience difficulties in accurately sensing the body’s oxygen levels due to reduced blood flow. As a result, the kidneys might produce more erythropoietin than necessary, leading to an overproduction of red blood cells and an increase in hemoglobin levels. This maladaptive response can further complicate the clinical management of CHF, as patients may develop polycythemia (an abnormally high red blood cell count).
Potential Risks of Elevated Hemoglobin in CHF
While the increase in hemoglobin levels in CHF is a compensatory mechanism, it can also have detrimental effects on the body. Elevated hemoglobin can lead to increased blood viscosity (thickness), which may cause further strain on the heart and exacerbate the symptoms of heart failure. Additionally, the increased blood viscosity may contribute to an increased risk of blood clots, which can lead to complications such as stroke or deep vein thrombosis (DVT).
Implications for Treatment and Management
Managing elevated hemoglobin in CHF requires careful monitoring and a balanced approach to treatment. If hemoglobin levels become excessively high, therapeutic interventions such as phlebotomy (removal of blood) or adjustments in erythropoiesis-stimulating agents may be necessary to reduce the risk of complications. Additionally, optimizing fluid management, correcting electrolyte imbalances, and addressing kidney function can help mitigate some of the contributing factors to elevated hemoglobin in CHF.
Conclusion
In summary, the increase in hemoglobin levels in individuals with congestive heart failure is primarily due to the body’s compensatory response to hypoxia. The kidneys release erythropoietin to stimulate the production of red blood cells, while fluid retention, dehydration, and autonomic nervous system activation also contribute to elevated hemoglobin levels. While this adaptation helps improve oxygen delivery, it can also have adverse effects, such as increased blood viscosity and a higher risk of clotting.
Related topics: